Your Personalized Exam May Include a Review of Current Health, Medical History and Family History to be Used for Personalized Treatment Options or Referrals that Meet Your Health Goals.
Women's Healthcare and Female Identified Persons
Evaluation, Treatment or Referral
Are You Ready for Pregnancy?
Preconception planning can help you and your partner understand how to boost your chances of a healthy pregnancy.

A preconception appointment is especially important if you’re over the age of 30 or you have any chronic health conditions or special concerns.
If possible, ask your partner to attend the preconception visit with you. Your partner’s health and lifestyle are important because they can affect both you and the baby. Healthy lifestyle choices before and during pregnancy are essential.

There’s more to the birds and the bees… apparently there’s environmental factors, diet, genetics and more. Discuss how you can plan a successful pregnancy.
Hormone Therapy
Hormone replacement therapy consists of medications containing female hormones to replace the ones the body no longer makes after menopause.
It is sometimes used to treat common menopausal symptoms, including hot flashes and vaginal discomfort.
Hormone therapy has also been proven to prevent bone loss and reduce fracture in postmenopausal women. Along with the benefits, there are risks associated with using hormone therapy. These risks depend on a few factors, including:
- the type of hormone therapy
- the dose
- how long the medication is taken
For best results, Goals Healthcare will create a hormone therapy tailored to You and re-evaluate your progress every month to be sure its benefits are still outweighing your risks.

Who should consider hormone therapy?
Despite its health risks, systemic estrogen is still an effective treatment for menopausal symptoms. The benefits of hormone therapy may outweigh the risks if you’re healthy and you:
- Experience moderate to severe hot flashes or other menopausal symptoms
- Have lost bone mass and either can’t tolerate or aren’t benefiting from other treatments
- Stopped having periods before age 40 (premature menopause) or lost normal function of your ovaries before age 40 (premature ovarian insufficiency)
Women who experience early menopause, particularly those who had their ovaries removed and don’t take estrogen therapy until at least age 45, have a higher risk of:
- Osteoporosis
- Heart disease
- Earlier death
- Parkinson’s-like symptoms (parkinsonism)
- Anxiety or depression
For women who reach menopause prematurely, the protective benefits of hormone therapy usually outweigh the risks. Your age, type of menopause and time since menopause play significant roles in the risks associated with hormone therapy.
Together we will prepare and plan throughout your menopausal (best) years.
Hot Flashes
Hot flashes are sudden feelings of warmth, which are usually most intense over the face, neck and chest.

People May Experience:
- Red skin
- Sweating
- Chills
Some Possible Treatments:
- Estrogen therapy is the most effective treatment option for relieving menopausal hot flashes. Depending on your personal and family medical history estrogen in the lowest dose and the shortest time frame needed to provide symptom relief for you may be needed. If you still have your uterus, you’ll need progestin in addition to estrogen.
- Low-dose antidepressants related to the class of drugs called selective serotonin and norepinephrine reuptake inhibitors (SNRIs and SSRIs) may decrease menopausal hot flashes. A low-dose antidepressant for management of hot flashes may be useful for women who can’t take estrogen for health reasons or for women who need an antidepressant for a mood disorder.
- Gabapentin (Neurontin, Gralise, others) is approved to treat seizures, but it has also been shown to help reduce hot flashes. This drug is useful in women who can’t use estrogen therapy and in those who also have nighttime hot flashes.
- Clonidine (Catapres, Kapvay, others) a pill or patch typically used to treat high blood pressure, might provide some relief from hot flashes.
- Natural Remedies
After Your comprehensive exam we will help plan Your long-term treatment Goals designed specifically for You.
Menopause
Menopause can be difficult. It requires treatments focused on relieving your signs and symptoms and preventing or managing chronic conditions that may occur with aging.
Menopause is often signaled by 12 months since your last menstruation.

People May Experience:
- Absence of menstruation
- Irregular menstruation
- Pain during sexual intercourse
- Whole body fatigue
- Night sweats
- Osteoporosis
- Hot flashes
- Sweating
- Sleep Issues
- Hair dryness
- Loss of scalp hair
- Anxiety
- Depression
- Irritability
- Moodiness
- Reduced sex drive
- Vaginal dryness
- Dry skin

Treatments May Include:
- Medications aimed at reducing the severity and frequency of hot flashes include estrogen, hormone therapy, venlafaxine and gabapentin.
- In some circumstances, oral hormone therapy may be prescribed.
- In some circumstances blood tests are recommended to check your level of Follicle-stimulating hormone (FSH) and estrogen (estradiol), because your FSH levels increase and estradiol levels decrease as menopause occurs.
- In some cases a thyroid-stimulating hormone (TSH) may be best, because an underactive thyroid (hypothyroidism) can cause symptoms similar to those of menopause.
- Natural Remedies
Treatments for Menopause that focus on symptomatic relief is a natural process. We are here to help You through the transition so You can remain Your Best Self, during Your Best Years.
Painful Urination (UTI)
Painful urination (dysuria) is discomfort or burning with urination, usually felt in the tube that carries urine out of your bladder (urethra) or the area surrounding your genitals (perineum).
A number of conditions can cause painful urination (dysuria). In women, urinary tract infections are a common cause of painful urination.
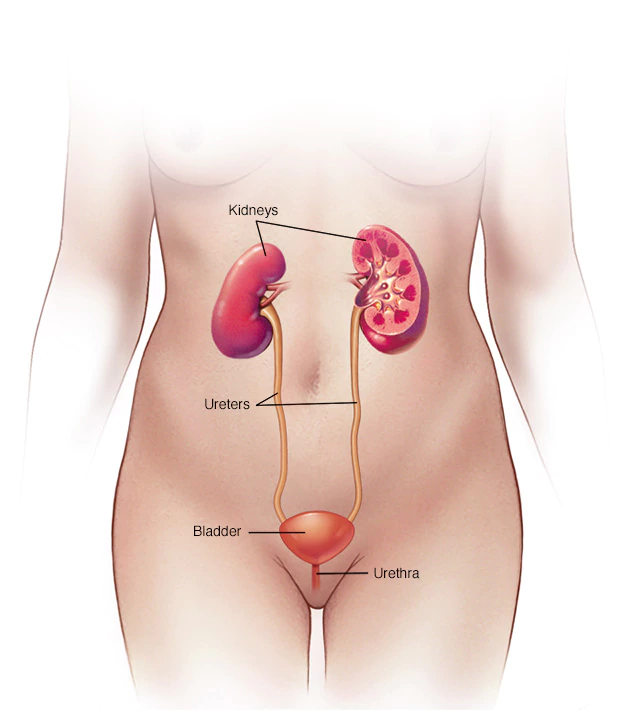
Conditions and factors that can cause painful urination may include:
- Bladder stones
- Chlamydia trachomatis
- Cystitis (bladder inflammation)
- Medications
- Genital herpes
- Gonorrhea
- Having a recent urinary tract procedure
- Urologic instruments for testing or treatment
- Kidney infection (pyelonephritis)
- Kidney stones
- Sexually transmitted diseases (STDs)
- Soaps, perfumes and other personal care products
- Urethral stricture (narrowing of the urethra)
- Urethritis (infection of the urethra)
- Urinary tract infection (UTI)
- Vaginitis (bacterial vaginosis)
- Yeast infection (vaginal)
Please make an appointment if:
- You have drainage or discharge from your vagina or change in vaginal discharge
- Your urine is foul-smelling or cloudy, or you see blood in your urine
- You have back pain or pain in your side (flank pain)
- You pass a kidney or bladder (urinary tract) stone
- A new persistent urge to urinate
- Involuntary loss of urine
- Pain or burning when urinating
- Pain in your back, side or groin
- Fever with urinary symptoms

Let’s get you back on the right (tract) track!
Polycystic Ovary Syndrome (PCOS)
PCOS is a hormonal disorder common among women of reproductive age. Women and female identified persons with PCOS may have infrequent or prolonged menstrual periods or excess male hormone (androgen) levels.
The ovaries may develop numerous small collections of fluid (follicles) and fail to regularly release eggs. The exact cause of PCOS is unknown. Early diagnosis and treatment along with weight loss may reduce the risk of long-term complications such as type 2 diabetes and heart disease.
Signs and symptoms of PCOS often develop around the time of the first menstrual period during puberty. Sometimes PCOS develops later, for example, in response to substantial weight gain.
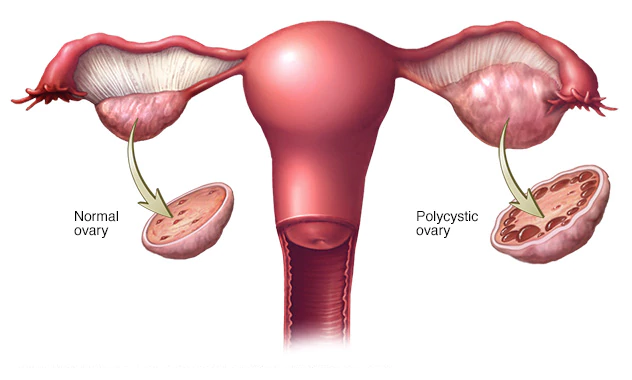
A diagnosis of PCOS is made when you experience at least two of these signs:
- Irregular periods
- Infrequent, irregular or prolonged menstrual cycles are the most common sign of PCOS.
- For example, you might have fewer than nine periods a year, more than 35 days between periods and abnormally heavy periods.
- Excess androgen. Elevated levels of male hormone may result in physical signs, such as excess facial and body hair (hirsutism), and occasionally severe acne and male-pattern baldness.
- Polycystic ovaries. Your ovaries might be enlarged and contain follicles that surround the eggs. As a result, the ovaries might fail to function regularly.
PCOS signs and symptoms are typically more severe if you’re obese.
Complications of PCOS can include:
- Infertility
- Gestational diabetes
- Pregnancy induced high blood pressure
- Miscarriage
- Premature birth
- Nonalcoholic steatohepatitis, a severe liver inflammation caused by fat accumulation in the liver
- Metabolic syndrome, a cluster of conditions including high blood pressure, high blood sugar, and abnormal cholesterol or triglyceride levels
- Type 2 diabetes
- Prediabetes
- Sleep apnea
- Depression, anxiety and eating disorders
- Abnormal uterine bleeding
- Cancer of the uterine lining (endometrial cancer)
We’ll work directly with You during every phase of being strong and beautiful.
STD and STI Screenings
Sexually transmitted diseases (STDs) and Sexually transmitted infections (STIs) are generally acquired by sexual contact. The organisms that cause sexually transmitted diseases may pass from person to person in blood, semen, or vaginal and other bodily fluids.

Sometimes these infections can be transmitted nonsexually, such as from mother to infant during pregnancy or childbirth, or through blood transfusions or shared needles.
It’s possible to contract sexually transmitted diseases from people who seem perfectly healthy, and who may not even be aware of the infection. STDs don’t always cause symptoms, which is one of the reasons experts prefer the term “sexually transmitted infections” to “sexually transmitted diseases.”
Sexually transmitted infections (STIs) can have a range of signs and symptoms, including no symptoms. That’s why they may go unnoticed until complications occur or a partner is diagnosed.
Signs and symptoms that might indicate an STI include:
- Sores or bumps on the genitals or in the oral or rectal area
- Painful or burning urination
- Discharge from the penis
- Unusual or odd-smelling vaginal discharge
- Unusual vaginal bleeding
- Pain during sex
- Sore, swollen lymph nodes, particularly in the groin but sometimes more widespread
- Lower abdominal pain
- Fever
- Rash over the trunk, hands or feet
Signs and symptoms may appear a few days after exposure, or it may take years before you have any noticeable problems, depending on the organism.
Because many people in the early stages of an STI experience no symptoms, screening for STIs is important in preventing complications.
Receive testing options while learning about several ways to reduce your risks and symptoms.
Unwanted Hair Growth (Hirsutism)
Hirsutism (HUR-soot-iz-um) is a condition of unwanted, male-pattern hair growth in women and female identified persons. Hirsutism results in excessive amounts of dark, coarse hair on body areas where men typically grow hair; face, chest and back.
The amount of body hair you have is largely determined by your genetic makeup. There’s a wide range of normal hair distribution, thickness and color due to differences in heredity. However, hirsutism is a medical condition that can arise from excess male hormones called androgens, primarily testosterone. It can also be due to a family trait.

When excessively high androgen levels cause hirsutism, other signs might develop over time, a process called Virilization. Signs of Virilization might include:
- Deepening voice
- Balding
- Acne
- Decreased breast size
- Increased muscle mass
- Enlargement of the clitoris
Although hirsutism can occur with no identifiable cause, with proper treatment, most symptoms can be treated.
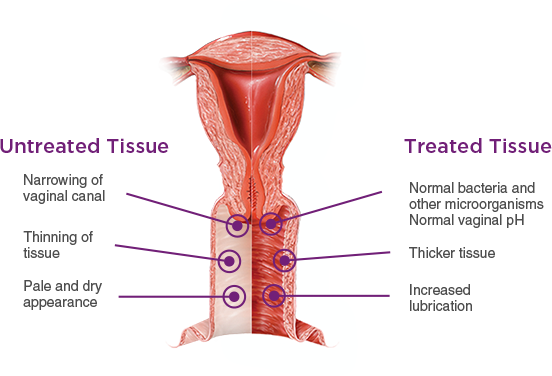
Vaginal Dryness
Vaginal dryness may be a problem for women and female identified persons at any age. It occurs more frequently when you’re older, particularly after menopause.
People May Experience:
- Intercourse discomfort
- Urinary discomfort
- Burning or itching
- Discharge
Some experience Vaginal atrophy (atrophic vaginitis) thinning, drying and inflammation of the vaginal walls due to your body having less estrogen. Vaginal atrophy occurs most often after menopause.

You may experience the following vaginal and urinary signs and symptoms:
- Vaginal dryness
- Vaginal burning
- Vaginal discharge
- Genital itching
- Burning with urination
- Urgency with urination
- More urinary tract infections
- Urinary incontinence
- Light bleeding after intercourse
- Discomfort with intercourse
- Decreased vaginal lubrication during sexual activity
- Shortening and tightening of the vaginal canal
Feeling better is right around the corner. Receive the help and treatment plan that’s right for You.
Vaginitis
Vaginitis is an inflammation of the vagina. The cause is usually a change in the normal balance of vaginal bacteria or an infection. Reduced estrogen levels after menopause and some skin disorders can also cause vaginitis.
People May Experience:
- Change in color
- Odor or discharge from vagina
- Vaginal itching or irritation
- Pain during intercourse
- Painful urination
- Light vaginal bleeding or spotting
The most common types of vaginitis are:
- Bacterial vaginosis, which results from a change of the normal bacteria found in your vagina to overgrowth of other organisms
- Yeast infections, which are usually caused by a naturally occurring fungus called Candida albicans
- Trichomoniasis, which is caused by a parasite and is commonly transmitted by sexual intercourse
Let’s do this together.
Men's Healthcare and Male Identified Persons
Evaluation, Treatment or Referral
Erectile Dysfunction
Erectile dysfunction (impotence) is the inability to get and keep an erection firm enough for sex.
Having erection trouble from time to time isn’t necessarily a cause for concern. If erectile dysfunction is an ongoing issue, however, it can cause stress, affect your self-confidence and contribute to relationship problems.
Problems getting or keeping an erection can also be a sign of an underlying health condition that needs treatment and a risk factor for heart disease.
Sometimes, treating an underlying condition is enough to reverse erectile dysfunction. In other cases, medications or other direct treatments can be used.
Some other erectile issues we can discuss include:
- You have concerns about your erections or you’re experiencing other sexual problems such as premature or delayed ejaculation
- You have diabetes, heart disease or another known health condition that might be linked to erectile dysfunction
- You have other symptoms along with erectile dysfunction
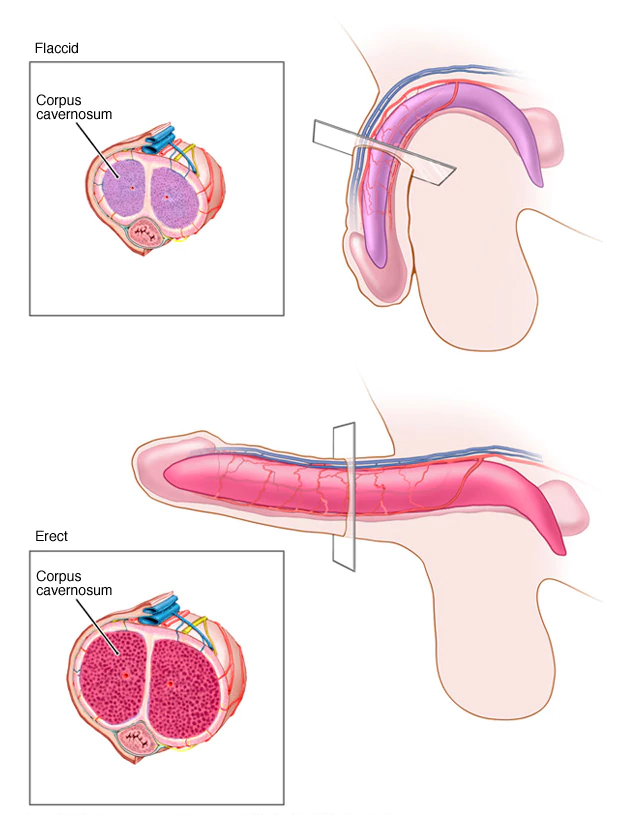
Male sexual arousal is a complex process that involves the brain, hormones, emotions, nerves, muscles and blood vessels. Erectile dysfunction can result from a problem with any of these. Likewise, stress and mental health concerns can cause or worsen erectile dysfunction. Sometimes a combination of physical and psychological issues causes erectile dysfunction.
Discrete consultations are available now through our telemedicine service.
Feel comfortable and confident discussing with us how to achieve peak performance because no one has time for erectile dysfunction!
Hormone Balancing
Hormone and testosterone therapy comes in many forms, such as creams, gels, patches or pills. A variety of factors will dictate whether hormones and testosterone therapy can be beneficial for you.
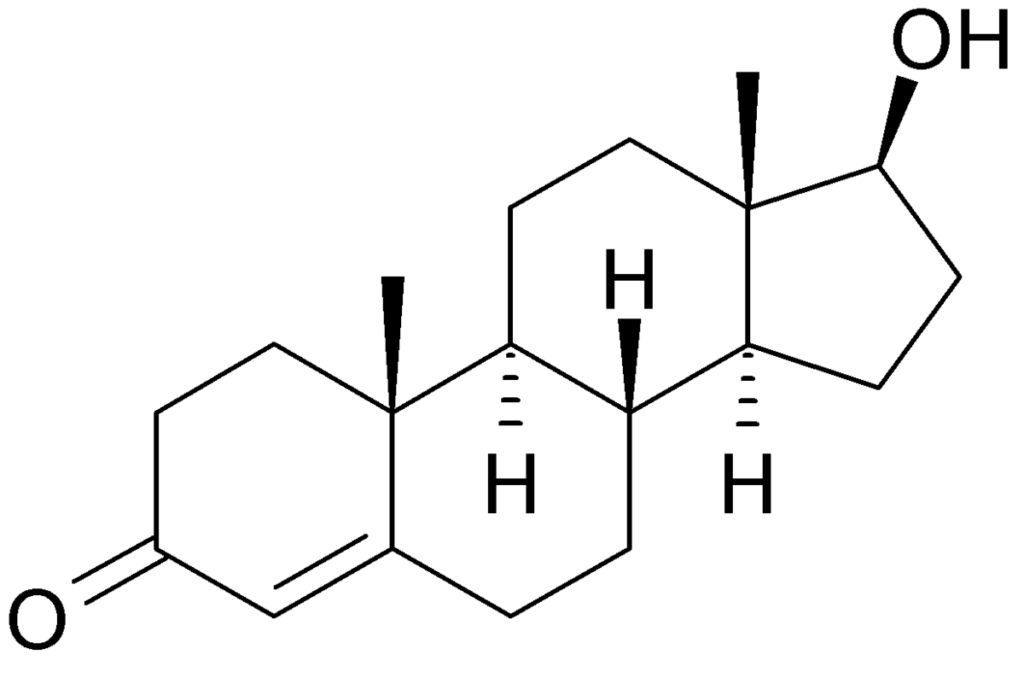
Testosterone therapy might be appropriate if
- You have reduced sex drive, depression and fatigue after surgically induced menopause, and estrogen therapy hasn’t relieved your symptoms
- You are postmenopausal, taking estrogen therapy and have a decreased sex drive with no other identifiable causes
- You mentally and physically do not feel like your adequate self

Learn if hormone and testosterone therapy is a good treatment option for You. Together we will find the best course of action designed for You.
MSM Screening
If you are sexually active, getting tested for STDs is one of the most important things you can do to protect your health and your partners. Feel comfortable having an open and honest conversation about your sexual history and STD testing with Dr. Levine. Find out if you should be tested. You owe it to yourself and your partner.

- All adults ages 18 to 64 should be tested at least once for HIV
- Screening at least once a year for syphilis, chlamydia, and gonorrhea for all sexually active gay, bisexual, and other men who have sex with men (MSM)
- MSM who have multiple or anonymous partners should be screened more frequently for STDs (3-to-6 month intervals)
- Sexually active gay and bisexual men may benefit from more frequent HIV testing (every 3 to 6 months).
- Anyone who has unsafe sex or shares injection drug equipment should get tested for HIV at least once a year.
Painful Urination (UTI)
Painful urination (dysuria) is discomfort or burning with urination, usually felt in the tube that carries urine out of your bladder (urethra) or the area surrounding your genitals (perineum).
A number of conditions can cause painful urination (dysuria). In male identified persons, urethritis and certain prostate conditions are frequent causes of painful urination.
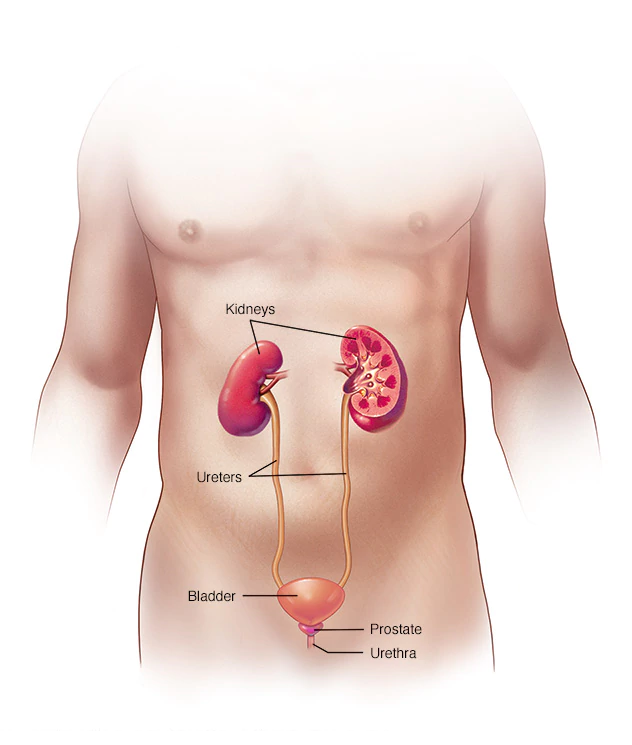
Conditions and factors that can cause painful urination may include
- Bladder stones
- Chlamydia trachomatis
- Cystitis (bladder inflammation)
- Medications
- Genital herpes
- Gonorrhea
- Having a recent urinary tract procedure
- Urologic instruments for testing or treatment
- Kidney infection (pyelonephritis)
- Kidney stones
- Sexually transmitted diseases (STDs)
- Soaps, perfumes and other personal care products
- Urethral stricture (narrowing of the urethra)
- Urethritis (infection of the urethra)
- Urinary tract infection (UTI)
Please make an appointment with Dr. Levine if
- You have drainage or discharge from your penis
- Your urine is foul-smelling or cloudy, or you see blood in your urine
- You have back pain or pain in your side (flank pain)
- You pass a kidney or bladder (urinary tract) stone
- A new persistent urge to urinate
- Involuntary loss of urine
- Pain or burning when urinating
- Pain in your back, side or groin
- Fever with urinary symptoms
Let’s get you back on the right (tract) track!
Prostate Screening
Cancer screening tests including the prostate-specific antigen (PSA) test is used to look for signs of prostate cancer. They can help identify cancer early on, when treatment is most effective. A normal PSA test, combined with a digital rectal exam, can help reassure you that it’s unlikely you have prostate cancer.
PSA screenings are generally encouraged in men between the ages of 45 and 70, and in men with an increased risk of prostate cancer.
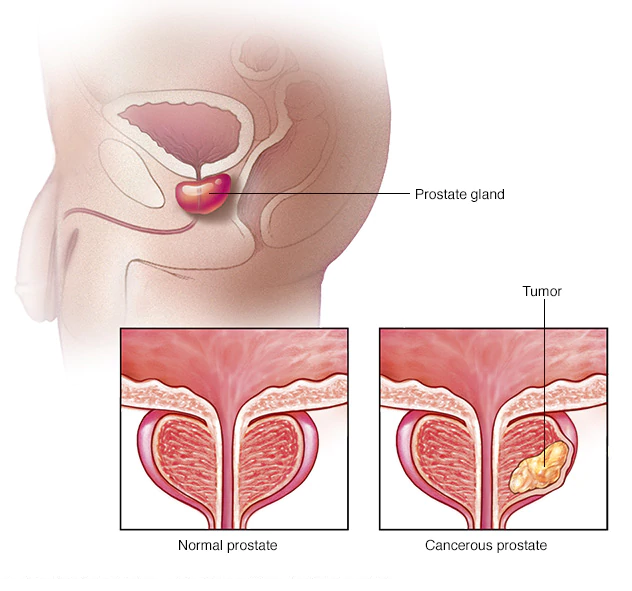
Prostate-specific antigen (PSA) is a protein produced by both cancerous (malignant) and noncancerous (benign) prostate tissue. PSA helps liquefy the semen. A small amount of PSA normally enters the bloodstream. Prostate cancer cells usually make more PSA than do benign cells, causing PSA levels in your blood to rise. But PSA levels can also be elevated in men with enlarged or inflamed prostate glands.
Besides the PSA number itself, we will consider a number of other factors
- Your age
- The size of your prostate gland
- How quickly your PSA levels are changing
- Whether you’re taking medications that affect PSA measurements
While high PSA levels can be a sign of prostate cancer, a number of conditions other than prostate cancer can cause PSA levels to rise.
Detecting certain types of prostate cancer early can be critical. Elevated PSA results may reveal prostate cancer that’s likely to spread to other parts of your body (metastasize), or they may reveal a quick-growing cancer that’s likely to cause other problems.
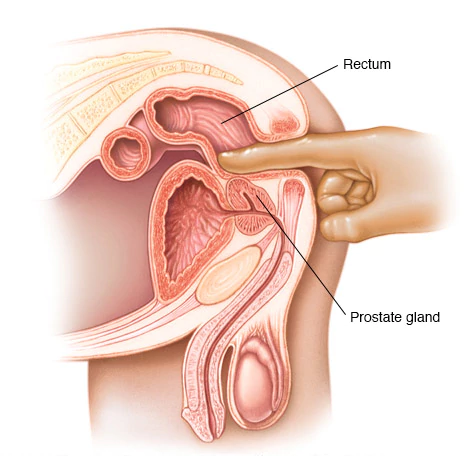
We will work with you for a comfortable and comprehensive cancer screening test along with a continued plan to remain on top of your prostate health.
STD and STI Screenings
Sexually transmitted diseases (STDs) and Sexually transmitted infections (STIs) are generally acquired by sexual contact. The organisms that cause sexually transmitted diseases may pass from person to person in blood, semen, or vaginal and other bodily fluids.

Sometimes these infections can be transmitted nonsexually, such as from mother to infant during pregnancy or childbirth, or through blood transfusions or shared needles.
It’s possible to contract sexually transmitted diseases from people who seem perfectly healthy, and who may not even be aware of the infection. STDs don’t always cause symptoms, which is one of the reasons experts prefer the term “sexually transmitted infections” to “sexually transmitted diseases.”
Sexually transmitted infections (STIs) can have a range of signs and symptoms, including no symptoms. That’s why they may go unnoticed until complications occur or a partner is diagnosed.
Signs and symptoms that might indicate an STI include:
- Sores or bumps on the genitals or in the oral or rectal area
- Painful or burning urination
- Discharge from the penis
- Unusual or odd-smelling vaginal discharge
- Unusual vaginal bleeding
- Pain during sex
- Sore, swollen lymph nodes, particularly in the groin but sometimes more widespread
- Lower abdominal pain
- Fever
- Rash over the trunk, hands or feet
Signs and symptoms may appear a few days after exposure, or it may take years before you have any noticeable problems, depending on the organism.
Because many people in the early stages of an STI experience no symptoms, screening for STIs is important in preventing complications.
Receiving testing options while learning about several ways to reduce your risk or keep symptoms from returning.
Mental Healthcare
Consultation, Diagnostics, Treatment or Referral
Anxiety
It’s normal to feel anxious from time to time, especially if your life is stressful (whose isn’t). However, excessive, ongoing anxiety and worry that are difficult to control and interfere with day-to-day activities may be a sign of generalized anxiety disorder.
Generalized anxiety disorder has symptoms that are similar to panic disorder, obsessive-compulsive disorder and other types of anxiety, but they’re all different conditions.
Living with generalized anxiety disorder can be a long-term challenge. In many cases, it occurs along with other anxiety or mood disorders.
In most cases, generalized anxiety disorder improves with psychotherapy and medications. Making lifestyle changes, learning coping skills and using relaxation techniques also can help.
Consultations are available in office and online using our telemedicine service online.
Bipolar
There are several types of bipolar and related disorders. They may include mania or hypomania and depression. Symptoms can cause unpredictable changes in mood and behavior, resulting in significant distress and difficulty in life. Symptoms can vary from person to person, and symptoms may vary over time.
Bipolar I disorder. You’ve had at least one manic episode that may be preceded or followed by hypomanic or major depressive episodes. In some cases, mania may trigger a break from reality (psychosis).
Bipolar II disorder. You’ve had at least one major depressive episode and at least one hypomanic episode, but you’ve never had a manic episode.
Cyclothymic disorder. You’ve had at least two years of many periods of hypomania symptoms and periods of depressive symptoms (though less severe than major depression).
Other types. These include, for example, bipolar and related disorders induced by certain drugs or alcohol or due to a medical condition, such as Cushing’s disease, multiple sclerosis or stroke.

Mania and hypomania are two distinct types of episodes, but they have the same symptoms. Mania is more severe than hypomania and causes more noticeable problems at work, school and social activities, as well as relationship difficulties. Mania may also trigger a break from reality (psychosis) and require hospitalization.
Manic and hypomanic episodes include three or more of these symptoms
- Abnormally upbeat, jumpy or wired
- Increased activity, energy or agitation
- Exaggerated sense of well-being and self-confidence (euphoria)
- Decreased need for sleep
- Unusual talkativeness
- Racing thoughts
- Distractibility
- Poor decision-making
A major depressive episode includes symptoms that are severe enough to cause noticeable difficulty in day-to-day activities, such as work, school, social activities or relationships.
An episode includes five or more of these symptoms
- Depressed mood, such as feeling sad, empty, hopeless or tearful (in children and teens, depressed mood can appear as irritability)
- Marked loss of interest or feeling no pleasure in all — or almost all — activities
- Significant weight loss when not dieting, weight gain, or decrease or increase in appetite (in children, failure to gain weight as expected can be a sign of depression)
- Either insomnia or sleeping too much
- Either restlessness or slowed behavior
- Fatigue or loss of energy
- Feelings of worthlessness or excessive or inappropriate guilt
- Decreased ability to think or concentrate, or indecisiveness
- Thinking about, planning or attempting suicide

The most prominent signs of bipolar disorder may include severe mood swings that are different from usual mood swings. Despite the mood extremes, people with bipolar disorder often don’t recognize how much their emotional instability disrupts their lives and the lives of their loved ones and don’t get the treatment they need.
And if you’re like some people with bipolar disorder, you may enjoy the feelings of euphoria and cycles of being more productive. However, this euphoria is always followed by an emotional crash that can leave you depressed, worn out and perhaps in financial, legal or relationship trouble.
Bipolar disorder doesn’t get better on its own. If you have any symptoms of depression or mania, please make an appointment with Dr. Levine or your mental health professional as soon as you can.
EMERGENCY HELP
If you have thoughts of hurting yourself, call 911 or your local emergency number immediately, go to an emergency room, or contact a trusted relative or friend.
Or call a suicide hotline number in the United States, call the National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255).
Consultations are available in office and online using our telemedicine app.
Depression
Depression causes a persistent feeling of sadness and loss of interest. It affects how you feel, think and behave and can lead to a variety of emotional and physical problems. You may have trouble doing normal day-to-day activities, and lose your desire for life.

Depression is not a weakness,
but you can’t simply “snap out” of it.
Depression will require long-term treatment. But don’t get discouraged. Together we will plan the best course of action suited for YOU.

For many people with depression, symptoms usually are severe enough to cause noticeable problems in day-to-day activities, such as work, school, social activities or relationships with others. Some people may feel generally miserable or unhappy without really knowing why.
Symptoms of depression may include
- Memory difficulties or personality changes
- Physical aches or pain
- Fatigue
- Loss of appetite
- Sleep problems
- Loss of interest in sex not caused by a medical condition or medication
- Suicidal thinking or feelings
If you think you feel depressed, please make an appointment with Dr. Levine or a mental health professional as soon as you can. If you’re reluctant to seek treatment, talk to a friend or loved one, any health care professional, a faith leader, or someone else you trust.
EMERGENCY HELP
If you have thoughts of hurting yourself, call 911 or your local emergency number immediately, go to an emergency room, or contact a trusted relative or friend.
Or call a suicide hotline number in the United States, call the National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255).
We can help you find ways to deal with your depression. No one has to live with the feeling of depression and Goals Healthcare is here to help you. Consultations are available in office and online using our telehealth.
Drug Addiction and Substance Abuse
is a disease that affects a person’s brain and behavior and leads to an inability to control the use of a legal or illegal substance, drug or medication. When you’re dependent, you may continue using the substance, drug or medication despite the harm it causes.
As time passes, you may need larger doses of the substance to feel the effects. Soon you may need it just to feel “normal” or “good” on a daily basis. As your use increases, you may find that it’s increasingly difficult to go without it. Attempts to stop use may cause intense cravings and make you feel physically ill (withdrawal symptoms).
If you feel you may have a substance use problem please find assistance. The sooner you seek help, the greater your chances for a long-term recovery.

EMERGENCY HELP
If you have thoughts of hurting yourself, call 911 or your local emergency number immediately, go to an emergency room, or contact a trusted relative or friend.
Or call a suicide hotline number in the United States, call the National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255).
Speak with Goals Healthcare or please see a mental health professional, such as an addiction psychiatrist, or a licensed alcohol and drug counselor.
Goals Healthcare will help you plan a course of action to beat your substance addiction. Together we will learn how to be our best selves every single day.
Consultations are available in office and online using our telemedicine app.
Family and Group Consultations
is a type of psychological consultation that can help family members and close groups improve communication and resolve conflicts.
Consultation plans are often short term. It may include all or some of the family members or group or just those able or willing to participate. Your consultation plan will be for Your situation.

Consultations may teach you skills and ways to set Goals to deepen family and group connections and get through stressful times. Consultations can occur before and after therapy sessions with your psychologist and psychiatrist.
Consultations are available in office and online using our telemedicine service online.
Grief Consultation
Losing a loved one is one of the most distressing and, unfortunately, common experiences people face. Most people experiencing normal grief and bereavement have a period of sorrow, numbness, and even guilt and anger. Gradually these feelings ease, and it’s possible to accept loss and move forward. For some people, feelings of loss are debilitating and don’t improve even after time passes.
This is known as complicated grief, sometimes called persistent complex bereavement disorder. In complicated grief, painful emotions are so long lasting and severe that you have trouble recovering from the loss and resuming your own life.
Different people follow different paths through the grieving experience. The order and timing of these phases may vary from person to person
- Accepting the reality of your loss
- Allowing yourself to experience the pain of your loss
- Adjusting to a new reality in which the deceased is no longer present
- Having other relationships
These differences are normal. But if you’re unable to move through these stages more than a year after the death of a loved one, you may have complicated grief.
During your consultations with Dr. Levine we will work to reclaim a sense of peace.

Counseling is available in office and online using our telemedicine service online.
Insomnia
is a common sleep disorder that can make it hard to fall asleep, hard to stay asleep, or cause you to wake up too early and not be able to get back to sleep. Insomnia can take away your energy level and mood but also your health, work performance and quality of life.
How much sleep is enough varies from person to person, but most adults need seven to eight hours a night. At some point, many adults experience short-term (acute) insomnia, which lasts for days or weeks. It’s usually the result of stress or a traumatic event.
Some people have long-term (chronic) insomnia that lasts for a month or more. Insomnia may be the primary problem, or it may be associated with other medical conditions or medications.

If insomnia makes it hard for you to function during the day, please make an appointment to identify the cause of your sleep problem and how it can be treated.
Medical Marijuana
Medical marijuana and natural sources of the cannabis plant have been used in healthcare for hundreds of years. As research continues on the use of marijuana for health care purposes we are learning more about the exact positive effects it may have for a variety of issues and conditions.

Goals Healthcare is certified in understanding the positive uses of medical marijuana and can prescribe for those who present any of the following:
- Post-Traumatic Stress Disorder (PTSD)
- Cancer
- Chronic Pain for More than 3 Months
- Inflammatory Bowel Disease (IBD) (Crohn’s or Ulcerative Colitis)
- Neuropathy
- Epilepsy
- Multiple Sclerosis (MS)
- Spinal Cord Damage with Spasticity
- Amyotrophic Lateral Sclerosis (ALS or Lou Gehrig’s disease)
- Parkinson’s Disease
- Huntington’s Disease
- HIV/AIDS
Memory Loss
A number of conditions not only Alzheimer’s disease can cause memory loss in older adults. Some degree of memory problems, as well as a modest decline in other thinking skills, is a fairly common part of aging. There’s a difference, however, between normal changes in memory and memory loss associated with Alzheimer’s disease and related disorders.

Normal age-related memory loss doesn’t prevent you from living a full, productive life. For example, you might occasionally forget a person’s name, but recall it later in the day. You might misplace your glasses sometimes. Or maybe you need to make lists more often than in the past to remember appointments or tasks.
These changes in memory are generally manageable and don’t disrupt your ability to work, live independently or maintain a social life.
Memory Loss and Dementia
The word “dementia” is an umbrella term used to describe a set of symptoms, including impairment in memory, reasoning, judgment, language and other thinking skills. Dementia usually begins gradually, worsens over time and impairs a person’s abilities in work, social interactions and relationships.
Often, memory loss that disrupts your life is one of the first or more-recognizable signs of dementia. Early signs might include
- Asking the same questions repeatedly
- Forgetting common words when speaking
- Mixing words up — saying “bed” instead of “table,” for exampleTaking longer to complete familiar tasks, such as following a recipe
- Misplacing items in inappropriate places, such as putting a wallet in a kitchen drawer
- Getting lost while walking or driving in a familiar area
- Having changes in mood or behavior for no apparent reason
Possible causes of reversible memory loss include
- Medications. Certain medications or a combination of medications can cause forgetfulness or confusion.
- Minor head trauma or injury. A head injury from a fall or accident even if you don’t lose consciousness can cause memory problems.
- Emotional disorders. Stress, anxiety or depression can cause forgetfulness, confusion, difficulty concentrating and other problems that disrupt daily activities.
- Alcoholism. Chronic alcoholism can seriously impair mental abilities. Alcohol can also cause memory loss by interacting with medications.
- Vitamin B-12 deficiency. Vitamin B-12 helps maintain healthy nerve cells and red blood cells. A vitamin B-12 deficiency common in older adults can cause memory problems.
- Hypothyroidism. An underactive thyroid gland (hypothyroidism) can result in forgetfulness and other thinking problems.
- Brain diseases. A tumor or infection in the brain can cause memory problems or other dementia-like symptoms.

Coming to terms with memory loss and the possible onset of dementia can be difficult. Some people try to hide memory problems, and some family members or friends compensate for a person’s loss of memory, sometimes without being aware of how much they’ve adapted to the impairment.
If you’re concerned about memory loss there are tests to determine the degree of memory impairment and diagnose the cause. Together, Goals will help plan the right course of action designed for You.
Consultations are available in-office and online using our telemedicine service.
Mental Health
It all starts from the top (our brain) and understanding our own mental health is critical to our overall physical well-being. We encourage all of our patients to discuss with us their mental health.

If you have any thoughts, concerns or questions about the following, please contact Goals Healthcare to discuss and learn more.
- Anxiety
- Depression
- Bipolar
- Grief Consultations
- Obsessive Compulsive Disorder (OCD)
- Insomnia and Sleep Hygiene
- PTSD
- Family and Group Consultations
- Sex Consultations
- Preconception Consultations
- Drug Addiction and Substance Abuse
- Memory Loss
- Weight Management
EMERGENCY HELP
If you have thoughts of hurting yourself, call 911 or your local emergency number immediately, go to an emergency room, or contact a trusted relative or friend.
Or call a suicide hotline number — in the United States, call the National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255).
Our mental health consultations are available in office and using our telemedicine service online. We can understand together, plan together, set Goals together and progress together.
Obsessive-Compulsive Disorder (OCD)
features a pattern of unreasonable thoughts and fears (obsessions) that lead you to do repetitive behaviors (compulsions). These obsessions and compulsions interfere with daily activities and cause significant distress.
You may or may not realize that your obsessions and compulsions are excessive or unreasonable, but they take up a great deal of time and interfere with your daily routine and social or work functioning. You may try to ignore or stop your obsessions, but that only increases your distress and anxiety. Ultimately, you feel driven to perform compulsive acts to try to ease your stress. Despite efforts to ignore or get rid of bothersome thoughts or urges, they keep coming back.
Obsessions often have themes to them, such as
-Fear of contamination or dirt
-Needing things orderly and symmetrical
-Aggressive or horrific thoughts about harming yourself or others
-Unwanted thoughts, including aggression, or sexual or religious subjects
If you have OCD, you do not have to be ashamed or embarrassed about the condition.
Treatment can be effective with personalized Goals and solutions. Consultations are available in office and online using our telemedicine app.
Panic Disorder (Panic Attacks)
A panic attack is a sudden episode of intense fear that triggers severe physical reactions when there is no real danger or apparent cause. When panic attacks occur, you might think you’re losing control, having a heart attack or even dying.
Many people have just one or two panic attacks in their lifetimes, and the problem goes away, perhaps when a stressful situation ends. But if you’ve had recurrent, unexpected panic attacks and spent long periods in constant fear of another attack, you may have a condition called panic disorder.
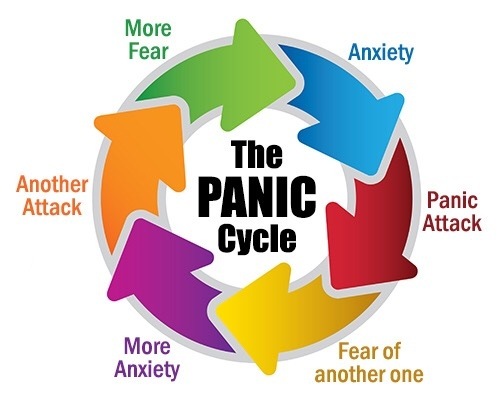
Although panic attacks themselves aren’t life-threatening, they can be frightening and significantly affect your quality of life. But treatment can be very effective.
One of the worst things about panic attacks is the intense fear that you’ll have another one. You may fear having panic attacks so much that you avoid certain situations where they may occur.
Panic attacks have many variations, but symptoms usually peak within minutes and include some of these signs or symptoms
- Sense of impending doom or danger
- Fear of loss of control or death
- Rapid, pounding heart rate
- Sweating
- Trembling or shaking
- Shortness of breath or tightness in your throat
- Chills
- Hot flashes
- Nausea
- Abdominal cramping
- Chest pain
- Headache
- Dizziness, lightheadedness or faintness
- Numbness or tingling sensation
- Feeling of unreality or detachment

Panic attacks are hard to manage on your own, and they may get worse without treatment. Panic attack symptoms can also resemble symptoms of other serious health problems, such as a heart attack, so it’s important to get evaluated if you aren’t sure what’s causing your symptoms.
There’s no sure way to prevent panic attacks or panic disorder. However, Goals Healthcare is uniquely qualified to help you find ways to plan, prevent and deal with each episode as best as possible.
Consultations are available in office and online using our telemedicine service online.
Post-Traumatic Stress Disorder (PTSD)
is a mental health condition that’s triggered by a terrifying event either experiencing it or witnessing it. Symptoms may include flashbacks, nightmares and severe anxiety, as well as uncontrollable thoughts about the event.
Most people who go through traumatic events may have temporary difficulty adjusting and coping, but with time and good self-care, they usually get better. If the symptoms get worse, last for months or even years, and interfere with your day-to-day functioning, you may have PTSD.
Getting effective treatment after PTSD symptoms develop can be critical to reduce symptoms and improve function.

Post-traumatic stress disorder symptoms may start within one month of a traumatic event, but sometimes symptoms may not appear until years after the event. These symptoms cause significant problems in social or work situations and in relationships. They can also interfere with your ability to go about your normal daily tasks.
PTSD symptoms are generally grouped into four types
- Intrusive memories
- Avoidance
- Negative changes in thinking and mood
- Changes in physical and emotional reactions
Symptoms can vary over time or vary from person to person.
You may have more PTSD symptoms when you’re stressed in general, or when you come across reminders of what you went through.
If you have disturbing thoughts and feelings about a traumatic event for more than a month, if they’re severe, or if you feel you’re having trouble getting your life back under control, talk with Dr. Levine or a mental health professional. Getting treatment as soon as possible can help prevent PTSD symptoms from getting worse.

EMERGENCY HELP
If you have thoughts of hurting yourself, call 911 or your local emergency number immediately, go to an emergency room, or contact a trusted relative or friend.
Or call a suicide hotline number — in the United States, call the National Suicide Prevention Lifeline at 1-800-273-TALK (1-800-273-8255).
Life can be tough, but we all deserve to feel our best. There are ways we can achieve this at Goals together. Let’s get started Today.
Consultations are available in office and online using our telemedicine service online.
Sex Consultations
Sex consultations can address concerns about sexual function, sexual feelings and intimacy, either individually or jointly with your partner. Sex counseling can be effective for individuals of any age, sex or sexual orientation.
Through sex consultations we can address issues such as
- Concerns about sexual desire or arousal
- Concerns about sexual interests or sexual orientation
- Impulsive sexual behavior
- Erectile dysfunction
- Ejaculating early (premature ejaculation)
- Difficulty with sexual arousal
- Trouble reaching orgasm (anorgasmia)
- Painful intercourse (dyspareunia)
- Intimacy issues related to a disability or chronic condition
- Concerns regarding past unwanted sexual experiences

Consultations are available in office and online using our telemedicine service online.
Let’s get you to peak performance!
Weight Management
Your weight is a balancing act, and calories are a major part of that equation. Weight comes down to how many calories you take in vs how many calories you burn.

You can do that by reducing extra calories from food and beverages, and increasing calories burned through physical activity.
While that seems simple, it can be challenging mentally and physically to get started.

Together we will implement a practical, effective and sustainable weight management plan. Goals Healthcare is here to assist throughout the process so you don’t have to do it alone. Receive weekly recipes, shopping lists, diet metrics and workout plans.

The key to successful weight management is a commitment to making changes Today. Talk with Goals Healthcare if you’re ready to get started.

Consultations, recipes, diets and workout plans are available in office and online using our telemedicine app.
Neurology and Clinical Neurophysiology
Consultation, Diagnostics, Treatment or Referral
ALS
ALS (Amyotrophic lateral sclerosis) is a progressive nervous system disease that affects nerve cells in the brain and spinal cord, causing loss of muscle control. ALS is often called Lou Gehrig’s disease, after the baseball player who was diagnosed with it. Doctors usually don’t know why ALS occurs. Some cases are inherited.
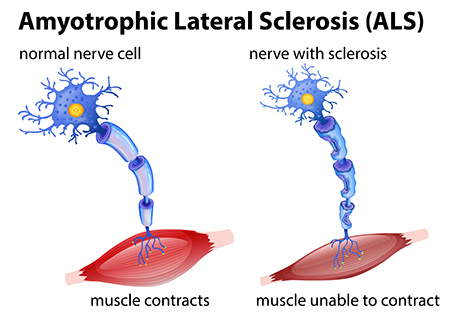
ALS often begins with muscle twitching and weakness in a limb, or slurred speech. Eventually, ALS affects control of the muscles needed to move, speak, eat and breathe.
Make an appointment with Goals Healthcare to have your ALS assessment and receive possible therapy options based on your specific needs.
Ataxia
Ataxia describes a lack of muscle control or coordination of voluntary movements, such as walking or picking up objects. A sign of an underlying condition, ataxia can affect various movements and create difficulties with speech, eye movement and swallowing.
Persistent ataxia usually results from damage to the part of your brain that controls muscle coordination (cerebellum).
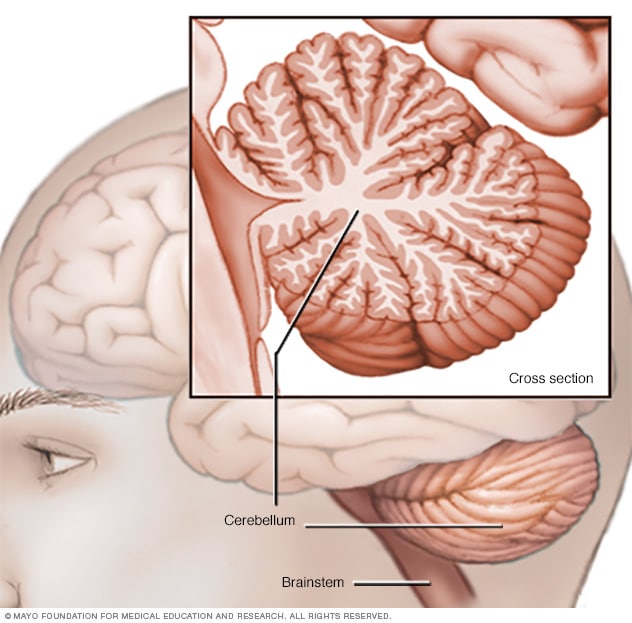
Many conditions can cause ataxia, including alcohol misuse, certain medication, stroke, tumor, cerebral palsy, brain degeneration and multiple sclerosis. Inherited defective genes also can cause the condition.
Treatments may be available based on the cause of Ataxia. Make an appointment with Goals Healthcare to have your symptoms reviewed.
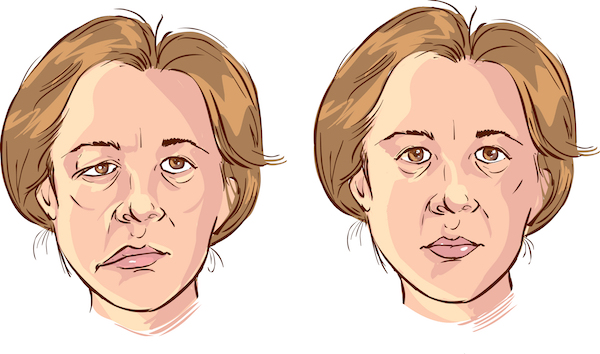
Bell's Palsy
The symptoms of Bell’s palsy include sudden weakness in your facial muscles. In most cases, the weakness is temporary and significantly improves over weeks. The weakness makes half of your face appear to droop. Your smile is one-sided, and your eye on that side resists closing.
Bell’s palsy, also known as acute peripheral facial palsy of unknown cause, can occur at any age. The exact cause is unknown. It’s believed to be the result of swelling and inflammation of the nerve that controls the muscles on one side of your face. Or it might be a reaction that occurs after a viral infection.
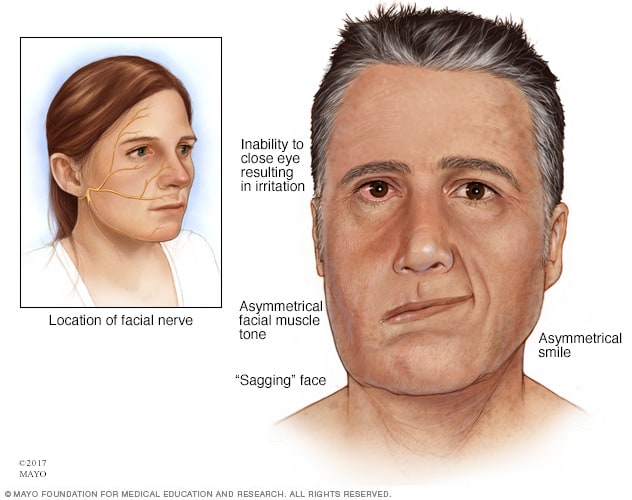
Bell’s palsy occurs more often in people who:
- Are pregnant, especially during the third trimester, or who are in the first week after giving birth
- Have an upper respiratory infection, such as the flu or a cold
- Have diabetes
An Electromyography (EMG) test can confirm the presence of nerve damage and determine its severity. An EMG measures the electrical activity of a muscle in response to stimulation and the nature and speed of the conduction of electrical impulses along a nerve.
Make an appointment with Goals Healthcare if you’re concerned about Bell’s palsy. Receive possible treatment options based on your individual needs.
Brachial Plexopathy (Peripheral Neuropathy)
Brachial plexopathy is a form of peripheral neuropathy. It occurs when there is damage to the brachial plexus. This is an area on each side of the neck where nerve roots from the spinal cord split into each arm’s nerves.
Symptoms may include:
- Recurrent burners and stingers
- Weakness in your hand or arm
- Neck pain
- Symptoms in both arms
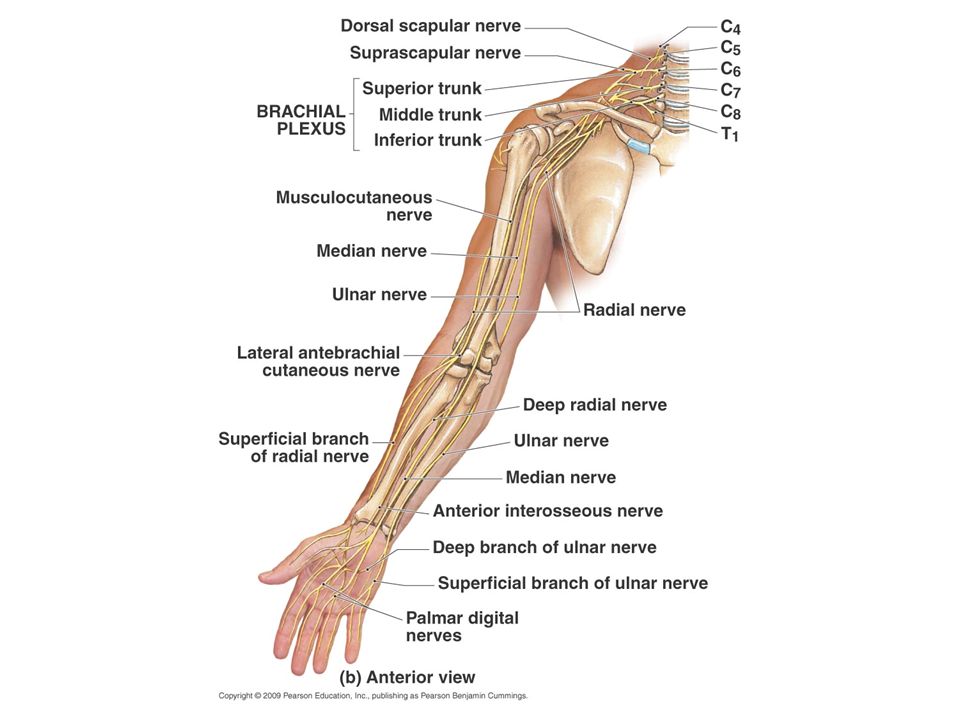
To help diagnose the extent and severity of a brachial plexus injury, you may have one of the following tests:
- Electromyography (EMG). During an EMG, a needle electrode is inserted through your skin into various muscles. The test evaluates the electrical activity of your muscles when they contract and when they’re at rest. You may feel a little pain when the electrodes are inserted, but most people can complete the test without much discomfort.
- Nerve conduction studies. These tests are usually performed as part of the EMG, and they measure the speed of conduction in your nerve when a small current passes through the nerve. This provides information about how well the nerve is functioning.
If you’re concerned with your symptoms make an appointment with Goals Healthcare today. Together, we will help plan the right course of action designed for You.
Carpel Tunnel Syndrome
Carpal Tunnel Syndrome is a condition where the main nerve that goes into the hand gets compressed in an area known as the carpal tunnel.
Carpal tunnel syndrome is caused by pressure on the median nerve. The carpal tunnel is a narrow passageway surrounded by bones and ligaments on the palm side of the hand. When the median nerve is compressed, symptoms can include numbness, tingling, and weakness in the hand and arm.

Carpal Tunnel is often indicated by a feeling of numbness and tingling in the fingertips. Patients sometimes experience their fingers going to sleep at night, causing them to awaken, and clumsiness of the hand.
The anatomy of the wrist, health problems and possibly repetitive hand motions can contribute to carpal tunnel syndrome.
To help diagnose the extent and severity of your injury, you may have one of the following tests:
- Electromyography (EMG). During an EMG, a needle electrode is inserted through your skin into various muscles. The test evaluates the electrical activity of your muscles when they contract and when they’re at rest. You may feel a little pain when the electrodes are inserted, but most people can complete the test without much discomfort.
- Nerve conduction studies. These tests are usually performed as part of the EMG, and they measure the speed of conduction in your nerve when a small current passes through the nerve. This provides information about how well the nerve is functioning.
Make an appointment with Goals Healthcare if you’re worried about symptoms affecting your daily life. Receive customized treatment options following your visit.
Chronic Migraine
Chronic Migraines can cause severe throbbing pain or a pulsing sensation and are often accompanied by nausea, vomiting, and extreme sensitivity to light and sound.
Migraine Attacks can last for hours to days, and the pain can be so severe that it interferes with your daily activities.

Migraines are often undiagnosed and untreated. If you regularly have signs and symptoms of migraine, keep a record of the attacks and how you treated them.
Make an appointment with Goals Healthcare to learn more about customized treatment options like Botox Injections for Chronic Migraines. Some insurance plans will cover a portion of or all costs associated with treatment if you qualify.
Chronic Migraine Injection Treatments
Botox Injections for Chronic Migraines may help limit severe migraine attacks and the pain that accompanies it.
How Does Botox for Chronic Migraines Work? Botox or botulinum toxin, gets into the small nerves that carry pain from the head to the brain, known as C-fibres.
Injections may reduce the amount of chemicals released from the nerve ending and therefore interrupts the feedback pathway that perpetuates migraine and headache.
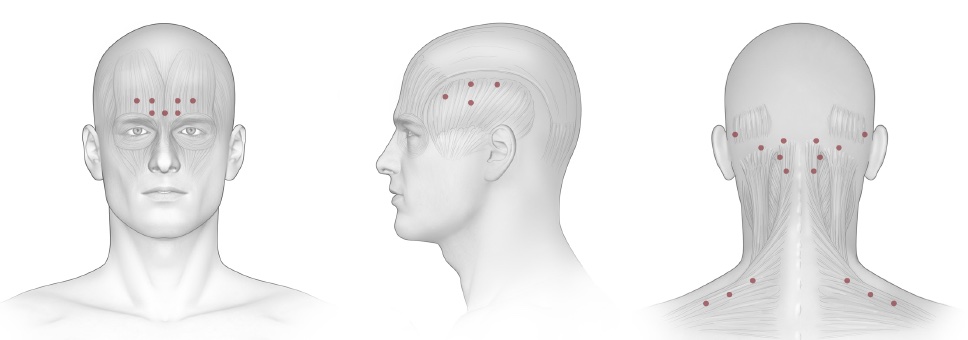
Migraines are often undiagnosed and untreated. If you regularly have signs and symptoms of migraine, keep a record of the attacks and how you treated them.
Botox is licensed for the treatment of chronic migraine, defined as 3 months of at least 15 days of headache a month, of which at least 8 days have migraine features, such as nausea, light or noise sensitivity, pulsating or lateralized pain.
Some insurance plans will cover a portion of or all costs associated with treatment. Make an appointment with Goals Healthcare to learn if Botox Injections for Chronic Migraines is right for you.
Dementia
Dementia is a term used to describe a group of symptoms affecting memory, thinking and social abilities severely enough to interfere with your daily life. It isn’t a specific disease, but several diseases can cause dementia.

Cognitive ChangesThough dementia generally involves memory loss, memory loss has different causes. Having memory loss alone doesn’t mean you have dementia, although it’s often one of the early signs of the condition.
Cognitive Changes
- Memory loss, which is usually noticed by someone else
- Difficulty communicating or finding words
- Difficulty with visual and spatial abilities, such as getting lost while driving
- Difficulty reasoning or problem-solving
- Difficulty handling complex tasks
- Difficulty with planning and organizing
- Difficulty with coordination and motor functions
- Confusion and disorientation
Psychological Changes
- Personality changes
- Depression
- Anxiety
- Inappropriate behavior
- Paranoia
- Agitation
- Hallucinations
If you’re concerned about dementia there are tests to determine the degree of memory impairment and diagnose the cause. Together, Goals Healthcare will help plan the right course of action designed for You.
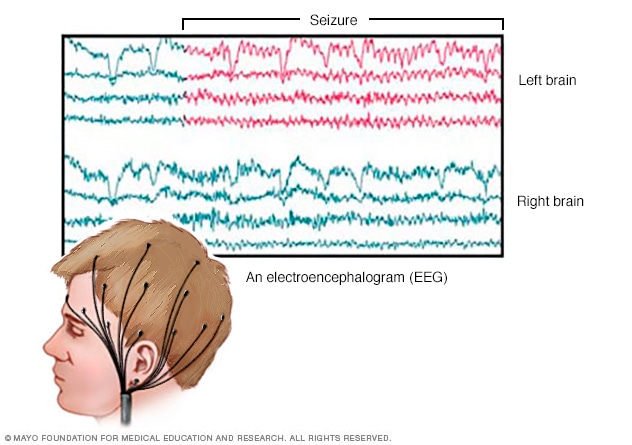
Electroencephalogram (EEG Test)
An Electroencephalogram (EEG Test) records the electrical activity of the brain via electrodes that are placed on the scalp. EEG results show changes in brain activity that may be useful in diagnosing brain conditions, especially epilepsy and other conditions that cause seizures.
What to expect during an EEG Test – Small discs will attach to your scalp fitted with electrodes. The electrodes are connected with wires to an instrument that amplifies the brain waves and records them on computer equipment. Once the electrodes are in place, an EEG typically takes between 20 and 40 minutes. During an EEG you’ll feel little or no discomfort. The electrodes don’t transmit any sensations. They just record your brain waves.
An EEG can find changes in brain activity that might also be helpful for diagnosing or treating:
- Brain tumors
- Brain damage from head injury
- Brain dysfunction that can have a variety of causes (encephalopathy)
- Sleep disorders
- Inflammation of the brain (herpes encephalitis)
- Stroke
- Sleep disorders
- Creutzfeldt-Jakob disease
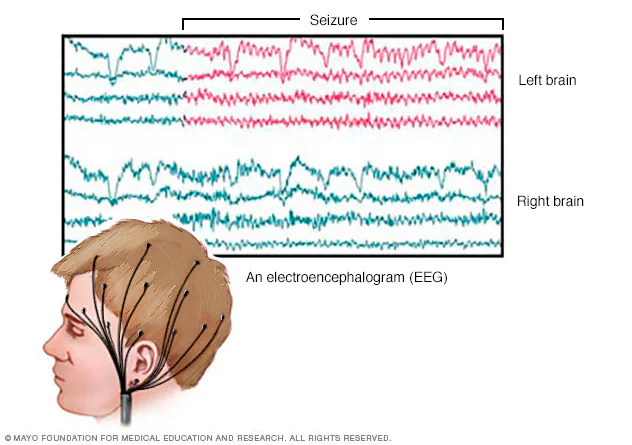
If you’re concerned about symptoms affecting your daily life make an appointment today. Goals Healthcare will help plan the right course of action designed for You.
Electromyography (EMG Test)
Electromyography (EMG) is a diagnostic procedure to assess the health of muscles and the nerve cells that control them (motor neurons). EMG results can reveal nerve dysfunction, muscle dysfunction or problems with nerve-to-muscle signal transmission.
What to expect during an EMG Test – During an EMG, a needle electrode is inserted through your skin into various muscles. The test evaluates the electrical activity of your muscles when they contract and when they’re at rest. You may feel a little pain when the electrodes are inserted, but most people can complete the test without much discomfort.
Nerve Conduction Studies are usually performed as part of the EMG and uses electrode stickers (surface electrodes) applied to the skin. They measure the speed of conduction in your nerve when a small current passes through the nerve. This provides information about how well the nerve is functioning.

If you’re concerned about symptoms affecting your daily life make an appointment today. Goals Healthcare will help plan the right course of action designed for You.
Encephalitis
Encephalitis is inflammation of the brain. There are several causes, but the most common is a viral infection.
Most people with viral encephalitis have mild flu-like symptoms, such as:
- Headache
- Fever
- Aches in muscles or joints
- Fatigue or weakness
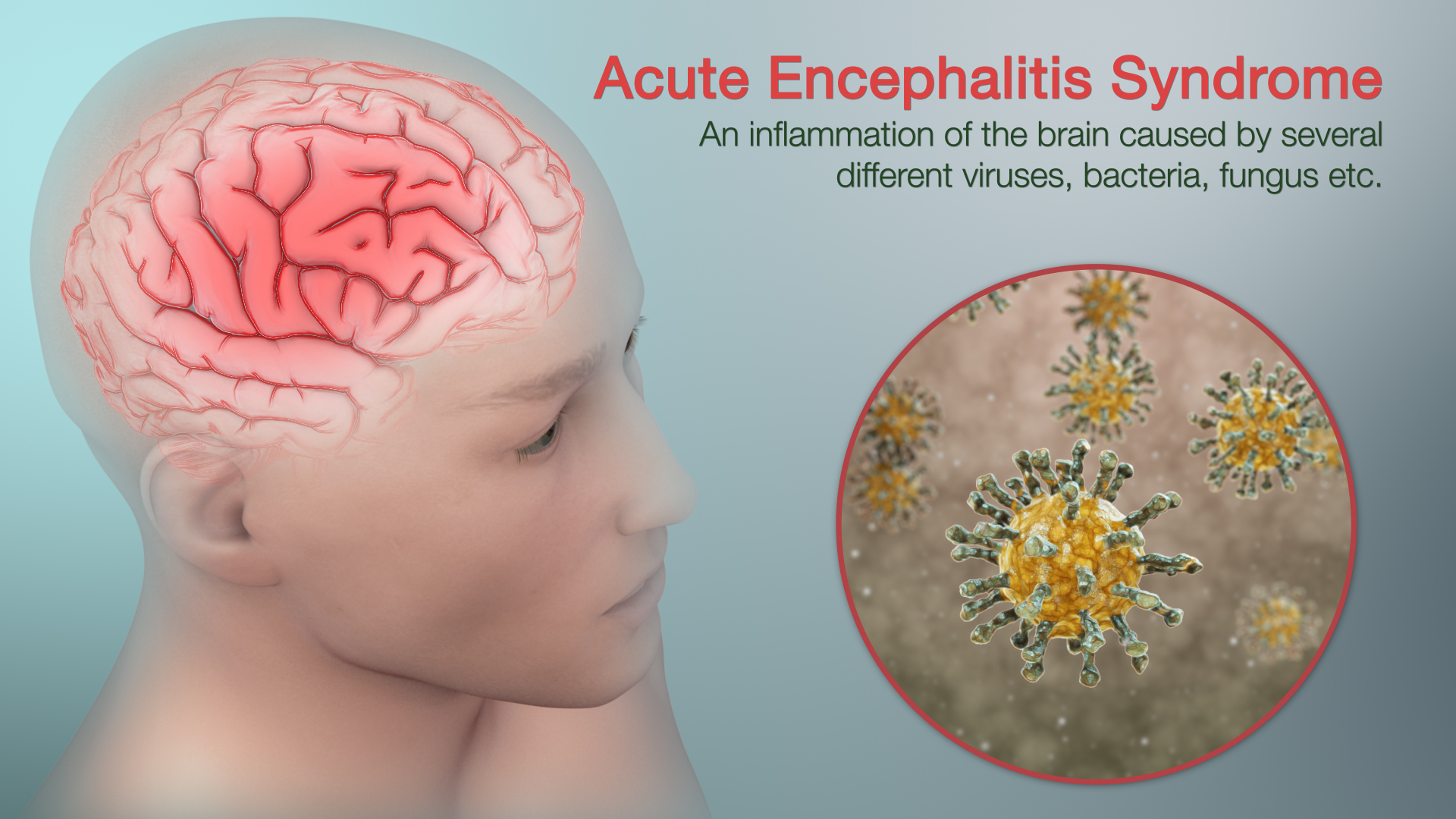
Sometimes the signs and symptoms are more severe, and might include:
- Confusion, agitation or hallucinations
- Seizures
- Loss of sensation or paralysis in certain areas of the face or body
- Muscle weakness
- Problems with speech or hearing
- Loss of consciousness (including coma)
If you’re concerned about symptoms affecting your daily life make an appointment today. Goals Healthcare will help plan the right course of action designed for You.
Epilepsy
Epilepsy is a central nervous system (neurological) disorder in which brain activity becomes abnormal, causing seizures or periods of unusual behavior, sensations and sometimes loss of awareness.
Because epilepsy is caused by abnormal activity in the brain, seizures can affect any process your brain coordinates. Seizure signs and symptoms may include:
- Temporary confusion
- A staring spell
- Stiff muscles
- Uncontrollable jerking movements of the arms and legs
- Loss of consciousness or awareness
- Psychological symptoms such as fear, anxiety or deja vu
If you’re concerned about symptoms affecting your daily life make an appointment today. Goals Healthcare will help plan the right course of action designed for You.
Guillain-Barré Syndrome
Guillain-Barre (gee-YAH-buh-RAY) syndrome is a rare disorder in which your body’s immune system attacks your nerves. Weakness and tingling in your extremities are usually the first symptoms.
The exact cause of Guillain-Barre syndrome is unknown. But two-thirds of patients report symptoms of an infection in the six weeks preceding. These include respiratory or a gastrointestinal infection or Zika virus.
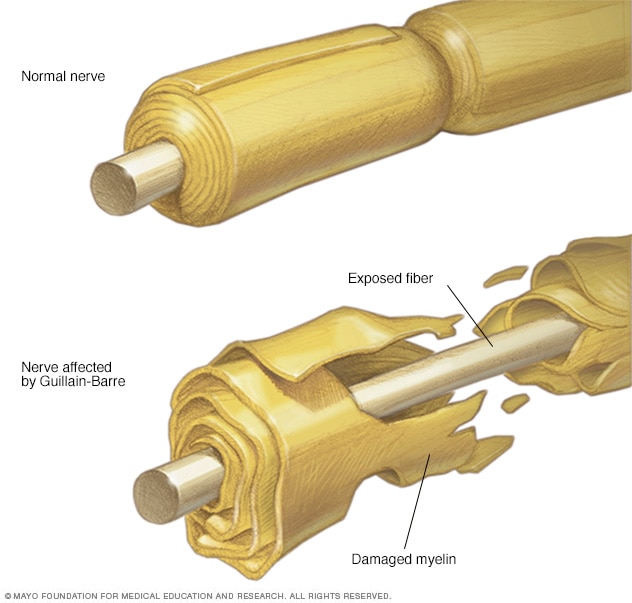
Signs and symptoms of Guillain-Barre syndrome may include:
- Prickling, pins and needles sensations in your fingers, toes, ankles or wrists
- Weakness in your legs that spreads to your upper body
- Unsteady walking or inability to walk or climb stairs
- Difficulty with facial movements, including speaking, chewing or swallowing
- Double vision or inability to move eyes
- Severe pain that may feel achy, shooting or cramplike and may be worse at night
- Difficulty with bladder control or bowel function
- Rapid heart rate
- Low or high blood pressure
- Difficulty breathing
There’s no known cure for Guillain-Barre syndrome, but several treatments can ease symptoms and reduce the duration of the illness.
If symptoms are affecting your daily life make an appointment today. Goals Healthcare is here to help customize the right course of action designed for You.
Headaches and Migraines
A tension headache, cluster headache or migraine can cause severe throbbing pain or a pulsing sensation, usually on one side of the head.
Migraines are often accompanied by nausea, vomiting, and extreme sensitivity to light and sound. Migraine attacks can last for hours to days, and the pain can be so severe that it interferes with your daily activities.

Migraines are often undiagnosed and untreated. If you regularly have signs and symptoms of migraine, keep a record of the attacks and how you treated them.
Make an appointment with Goals Healthcare to have your symptoms reviewed and receive personalized treatment options like Botox Injections for Chronic Migraines. Some insurance plans will cover a portion of or all costs associated with treatment if you qualify.
Head Injury
A mild traumatic brain injury may affect your brain cells temporarily. More-serious traumatic brain injury can result in bruising, torn tissues, bleeding and other physical damage to the brain. These injuries can result in long-term complications and should be checked immediately.
Traumatic brain injury can have wide-ranging physical and psychological effects. Some signs or symptoms may appear immediately after the traumatic event, while others may appear days or weeks later.

The signs and symptoms of mild traumatic brain injury may include:
- Headache
- Nausea or vomiting
- Fatigue or drowsiness
- Problems with speech
- Dizziness or loss of balance
- Sensory problems, such as blurred vision, ringing in the ears, a bad taste in the mouth or changes in the ability to smell
- Sensitivity to light or sound
- Loss of consciousness for a few seconds to a few minutes
- No loss of consciousness, but a state of being dazed, confused or disoriented
- Memory or concentration problems
- Mood changes or mood swings
- Feeling depressed or anxious
- Difficulty sleeping
- Sleeping more than usual
Moderate to severe traumatic brain injuries can include any of the signs and symptoms of mild injury, as well as these symptoms that may appear within the first hours to days after a head injury:
- Loss of consciousness from several minutes to hours
- Persistent headache or headache that worsens
- Repeated vomiting or nausea
- Convulsions or seizures
- Dilation of one or both pupils of the eyes
- Clear fluids draining from the nose or ears
- Inability to awaken from sleep
- Weakness or numbness in fingers and toes
- Loss of coordination
- Profound confusion
- Agitation, combativeness or other unusual behavior
- Slurred speech
- Coma and other disorders of consciousness
If you experienced a head injury and are concerned make an appointment today.
Loss of Feeling
Loss of Feeling or Numbness is most often caused by damage, irritation or compression of nerves.
A single nerve branch, or several nerves, may be affected, as with a slipped disc in the back or carpal tunnel syndrome in the wrist.
Certain diseases, such as diabetes, which can damage the longest, most sensitive nerve fibers (such as those going to your feet), can also cause numbness.

If your loss of feeling or numbness is getting in the way of your daily life, causing pain and not going away please contact Goals Healthcare to diagnose and treat the issue as soon as possible. A variety of tests may be needed to confirm the cause before appropriate treatment can begin.
Memory Loss
A number of conditions not only Alzheimer’s disease can cause memory loss in adults. Some degree of memory problems, as well as a modest decline in other thinking skills, is a fairly common part of aging. There’s a difference, however, between normal changes in memory and memory loss associated with Alzheimer’s disease and related disorders.

Normal age-related memory loss doesn’t prevent you from living a full, productive life. For example, you might occasionally forget a person’s name, but recall it later in the day. You might misplace your glasses sometimes. Or maybe you need to make lists more often than in the past to remember appointments or tasks.
These changes in memory are generally manageable and don’t disrupt your ability to work, live independently or maintain a social life.
Memory Loss and Dementia
The word “dementia” is an umbrella term used to describe a set of symptoms, including impairment in memory, reasoning, judgment, language and other thinking skills. Dementia usually begins gradually, worsens over time and impairs a person’s abilities in work, social interactions and relationships.
Often, memory loss that disrupts your life is one of the first or more-recognizable signs of dementia. Early signs might include
- Asking the same questions repeatedly
- Forgetting common words when speaking
- Mixing words up saying “bed” instead of “table,” for example Taking longer to complete familiar tasks, such as following a recipe
- Misplacing items in inappropriate places, such as putting a wallet in a kitchen drawer
- Getting lost while walking or driving in a familiar area
- Having changes in mood or behavior for no apparent reason
Possible causes of reversible memory loss include
- Medications. Certain medications or a combination of medications can cause forgetfulness or confusion.
- Minor head trauma or injury. A head injury from a fall or accident even if you don’t lose consciousness can cause memory problems.
- Emotional disorders. Stress, anxiety or depression can cause forgetfulness, confusion, difficulty concentrating and other problems that disrupt daily activities.
- Alcoholism. Chronic alcoholism can seriously impair mental abilities. Alcohol can also cause memory loss by interacting with medications.
- Vitamin B-12 deficiency. Vitamin B-12 helps maintain healthy nerve cells and red blood cells. A vitamin B-12 deficiency common in older adults can cause memory problems.
- Hypothyroidism. An underactive thyroid gland (hypothyroidism) can result in forgetfulness and other thinking problems.
- Brain diseases. A tumor or infection in the brain can cause memory problems or other dementia-like symptoms.

If you’re concerned about memory loss there are tests to determine the degree of memory impairment and diagnose the cause. Together, Goals Healthcare will help plan the right course of action designed for You.
Muscular Dystrophy
Muscular dystrophy is a group of diseases that cause progressive weakness and loss of muscle mass. In muscular dystrophy, abnormal genes (mutations) interfere with the production of proteins needed to form healthy muscle.
There’s no cure for muscular dystrophy. But medications and therapy can help manage symptoms and slow the course of the disease.
The main sign of muscular dystrophy is progressive muscle weakness. Specific signs and symptoms begin at different ages and in different muscle groups, depending on the type of muscular dystrophy.
Signs and symptoms, which typically appear in early childhood, might include:
- Frequent falls
- Difficulty rising from a lying or sitting position
- Trouble running and jumping
- Waddling gait
- Walking on the toes
- Large calf muscles
- Muscle pain and stiffness
- Learning disabilities
- Delayed growth
Goals Healthcare is here to help along your health journey. Book your appointment today to discuss your customized plan of action.
Myasthenia Gravis
Myasthenia gravis (my-us-THEE-nee-uh GRAY-vis) is characterized by weakness and rapid fatigue of any of the muscles under your voluntary control. It’s caused by a breakdown in the normal communication between nerves and muscles.
Muscle weakness caused by myasthenia gravis worsens as the affected muscle is used. Because symptoms usually improve with rest, muscle weakness can come and go. However, the symptoms tend to progress over time, usually reaching their worst within a few years after the onset of the disease.
In more than half of people who develop myasthenia gravis, their first signs and symptoms involve eye problems, such as:
- Drooping of one or both eyelids (ptosis)
- Double vision (diplopia), which may be horizontal or vertical, and improves or resolves when one eye is closed
Myasthenia gravis can also cause weakness in your neck, arms and legs. Weakness in your legs can affect how you walk. Weak neck muscles make it hard to hold up your head. Symptoms can include difficulty:
- Breathing
- Seeing
- Swallowing
- Chewing
- Walking
- Using your arms or hands
- Holding up your head
Book an appointment today if you’re concerned about Myasthenia Gravis symptoms. Goals Healthcare can help plan the right course of action designed for You.
Myopathy
Myopathies are rare muscle diseases mostly present at birth (congenital myopathies) that result from genetic defects. There are many different types of congenital myopathies, but most share common features, including lack of muscle tone and weakness.
Common signs and symptoms include:
- Lack of muscle tone
- Muscle weakness
- Delayed motor skills
- Noticeable facial weakness
- Drooping eyelids
- Muscle cramps or contractions
There are different types of congenital myopathies, some of which include:
- Central core disease. This condition causes muscle weakness and developmental problems. Some people may develop a significant reaction to general anesthesia (malignant hyperthermia).
- Centronuclear myopathies. These rare conditions cause muscle weakness in the face, arms, legs and eye muscles, and breathing problems.
- Congenital fiber type disproportion myopathy. Small fibers are found on muscle tissue during a biopsy. This condition causes muscle weakness in the face, neck, arms, legs and trunk.
- Nemaline myopathy. Nemaline myopathy is one of the more common congenital myopathies and causes muscle weakness in the face, neck, arms and legs, and sometimes scoliosis. It may also cause breathing and feeding problems.
- Multiminicore disease. This condition has several subtypes and often causes severe muscle weakness in the arms and legs, and scoliosis.
- Myotubular myopathy. This rare condition, which occurs only in males, causes muscle weakness, floppiness and breathing problems.
- Other myopathies. Other rare myopathies include autophagic vacuolar myopathy, cap disease, congenital myopathy with arrest of myogenesis, myosin storage (hyaline body) myopathy and zebra body myopathy.

Goals Healthcare is here to help along your health journey. Book an appointment today if you’re concerned about symptoms affecting your daily life.
Occipital Nerve Block (Base of the Head)
An occipital nerve block may provide temporary pain relief for certain headache disorders, like occipital neuralgia and cluster headaches. It can also help with neck and head pain related to injuries, such as whiplash.
Occipital neuralgia can affect anyone. You may be more likely to suffer from occipital neuralgia if you have:
- Degenerative disk disease
- Diabetes
- Gout
- Osteoarthritis of your upper spine
- Vasculitis (blood vessel inflammation)
What to expect during Nerve Block Injections
- An Occipital Nerve Block is an injection of medication close to a targeted nerve or group of nerves.
- Injections are placed into the base of the skull to block pain signals from the nerves.
- The medicine goes into an area around a nerve known as the occipital nerve.
- An injection of anti-inflammatory medication in addition to local anesthetic may allow the damaged nerves to heal by relieving the inflammation.
- The goal of treatment is to decrease and prevent additional nerve pain. Some injections provide prolonged pain relief.
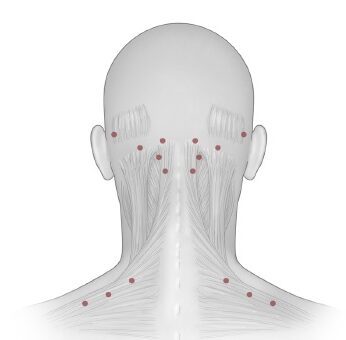
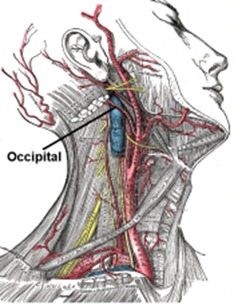
If you regularly have signs and symptoms of nerve pain, keep a record of the pain and how you treated it.
Some insurance plans will cover a portion of or all costs associated with treatment. Make an appointment with Goals Healthcare to learn if Nerve Blocks are right for you.
Nerve Conduction Studies
Nerve Conduction Studies are usually performed as part of the Electromyography (EMG). It uses electrode stickers (surface electrodes) applied to the skin to measure the speed of conduction in your nerve when a small current passes through. This provides information about how well the nerve is functioning.
Electromyography (EMG) is a diagnostic procedure to assess the health of muscles and the nerve cells that control them (motor neurons). EMG results can reveal nerve dysfunction, muscle dysfunction or problems with nerve-to-muscle signal transmission.
What to expect during an EMG Test – During an EMG, a needle electrode is inserted through your skin into various muscles. The test evaluates the electrical activity of your muscles when they contract and when they’re at rest. You may feel a little pain when the electrodes are inserted, but most people can complete the test without much discomfort.

If you’re concerned about symptoms affecting your daily life make an appointment today. Goals Healthcare will help plan the right course of action designed for You.
Neuropathy
Neuropathy is a result of damage to the nerves located outside of the brain and spinal cord (peripheral nerves), often causes weakness, numbness and pain, usually in the hands and feet. It can also affect other areas and body functions including digestion, urination and circulation.
Your peripheral nervous system sends information from your brain and spinal cord (central nervous system) to the rest of your body. The peripheral nerves also send sensory information to the central nervous system.
Peripheral neuropathy can result from traumatic injuries, infections, metabolic problems, inherited causes and exposure to toxins. One of the most common causes is diabetes.

Signs and symptoms of peripheral neuropathy might include:
- Gradual onset of numbness, prickling or tingling in your feet or hands, which can spread upward into your legs and arms
- Sharp, jabbing, throbbing or burning pain
- Extreme sensitivity to touch
- Pain during activities that shouldn’t cause pain, such as pain in your feet when putting weight on them or when they’re under a blanket
- Lack of coordination and falling
- Muscle weakness
- Feeling as if you’re wearing gloves or socks when you’re not
- Paralysis if motor nerves are affected
If autonomic nerves are affected, signs and symptoms might include:
- Heat intolerance
- Excessive sweating or not being able to sweat
- Bowel, bladder or digestive problems
- Drops in blood pressure, causing dizziness or lightheadedness
If you’re concerned with your signs and symptoms make an appointment with Goals Healthcare today. Together, we will help plan the right course of action designed for You.
Parkinson's Disease
Parkinson’s disease is a progressive nervous system disorder that affects movement. Symptoms start gradually, sometimes starting with a barely noticeable tremor in just one hand. Tremors are common, but the disorder also commonly causes stiffness or slowing of movement.
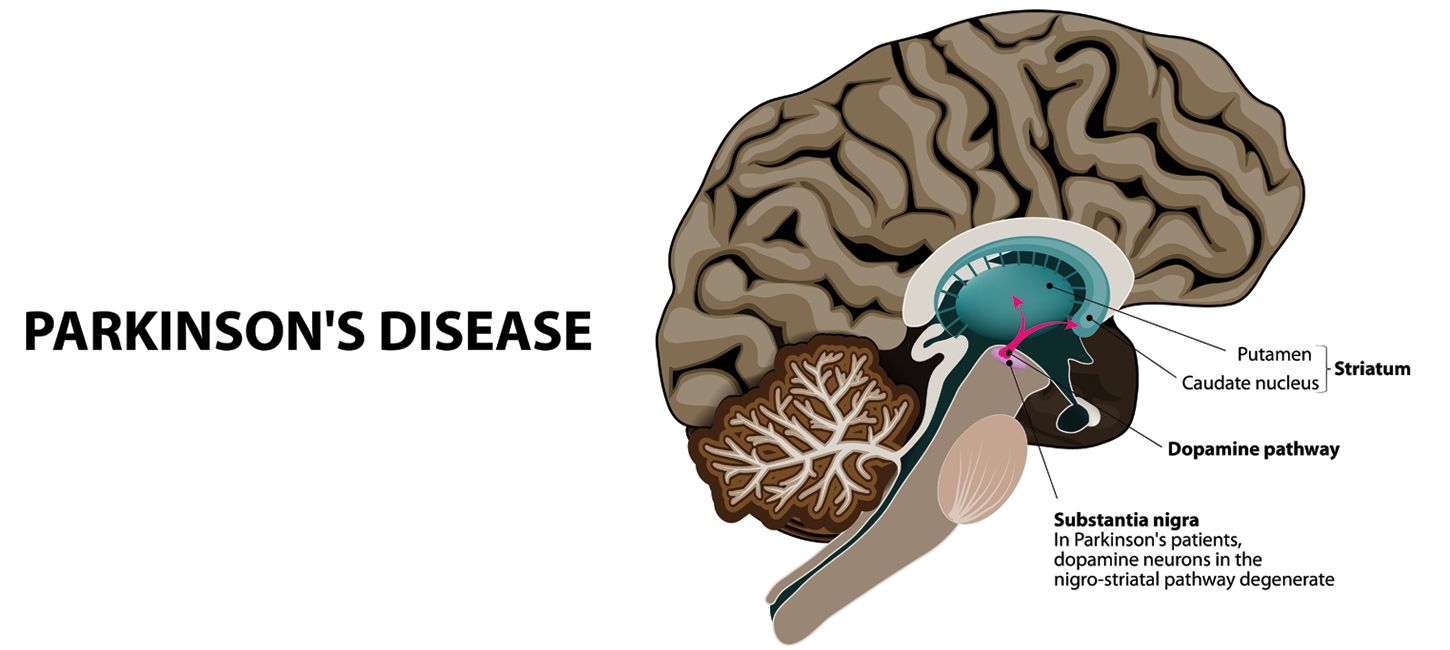
Parkinson’s signs and symptoms may include:
- Tremor. A tremor, or shaking, usually begins in a limb, often your hand or fingers. You may rub your thumb and forefinger back and forth, known as a pill-rolling tremor. Your hand may tremble when it’s at rest.
- Slowed movement (bradykinesia). Over time, Parkinson’s disease may slow your movement, making simple tasks difficult and time-consuming. Your steps may become shorter when you walk. It may be difficult to get out of a chair. You may drag your feet as you try to walk.
- Rigid muscles. Muscle stiffness may occur in any part of your body. The stiff muscles can be painful and limit your range of motion.
- Impaired posture and balance. Your posture may become stooped, or you may have balance problems as a result of Parkinson’s disease.
- Loss of automatic movements. You may have a decreased ability to perform unconscious movements, including blinking, smiling or swinging your arms when you walk.
- Speech changes. You may speak softly, quickly, slur or hesitate before talking. Your speech may be more of a monotone rather than have the usual inflections.
- Writing changes. It may become hard to write, and your writing may appear small.
If you’re concerned about symptoms affecting your daily life make an appointment today. Together, we will help plan the right course of action designed for You.
Seizures
A seizure is a sudden, uncontrolled electrical disturbance in the brain. It can cause changes in your behavior, movements or feelings, and in levels of consciousness.
Seizure signs and symptoms may include:
- Temporary confusion
- A staring spell
- Stiff muscles
- Uncontrollable jerking movements of the arms and legs
- Loss of consciousness or awareness
- Psychological symptoms such as fear, anxiety or deja vu
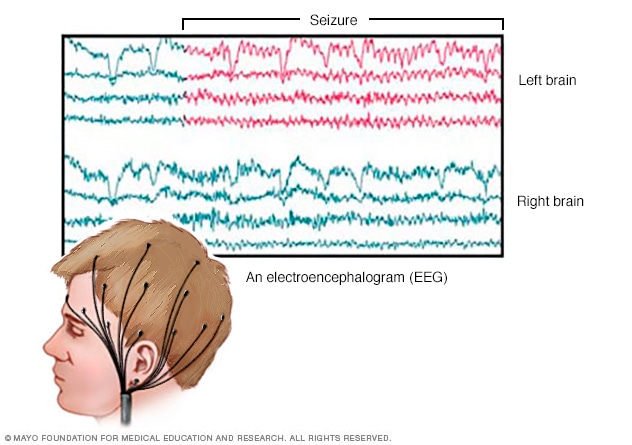
Having two or more seizures at least 24 hours apart that aren’t brought on by an identifiable cause is generally considered to be epilepsy. Epilepsy is a central nervous system (neurological) disorder.
If you’re concerned about seizures affecting your daily life make an appointment today. Goals Healthcare will help plan the right course of action designed for You.
Skin Biopsy for Small Fiber Neuropathy
A skin biopsy for Small Fiber Neuropathy is a procedure to remove cells from the surface of your body so that they can be tested in a lab. It is most often used to diagnose skin conditions and diseases, including:
- Neuropathy
- Numbness
- Tingling
- Pain
- Sensory Symptoms
Shave biopsy – During a shave biopsy, a tool like a razor is used to scrape the surface of the skin. The goal is to remove irregular tissue to send to the lab. Stitches usually aren’t needed after this procedure.
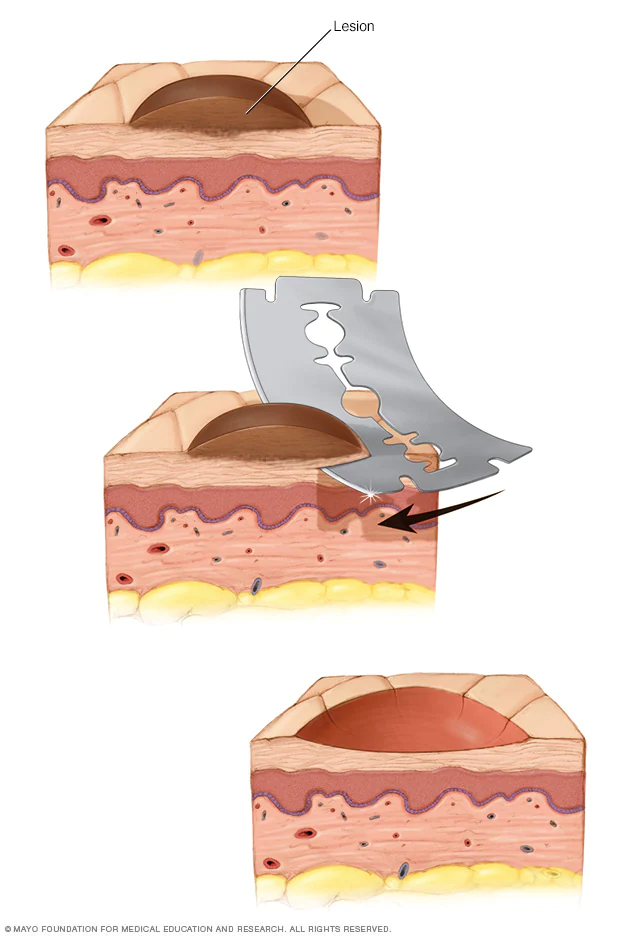
Punch biopsy – During a punch biopsy, a round-tipped cutting tool is used to remove deeper layers of skin for testing. Depending on the size, stitches may be needed to close the wound.
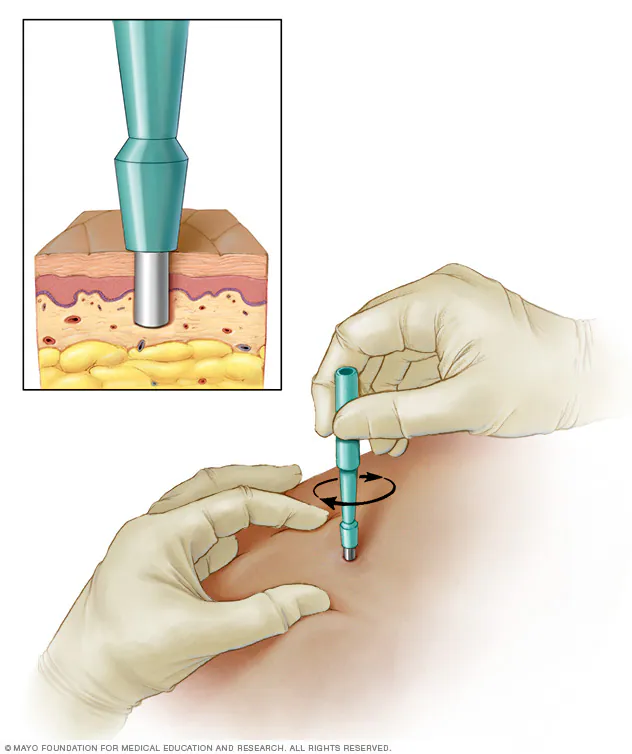
If you’re concerned about symptoms affecting your daily life make an appointment today. Goals Healthcare will help plan the right course of action designed for You.
Spinal Pain
A spinal cord injury is damage to any part of the spinal cord or nerves at the end of the spinal canal. It can cause permanent changes in strength, sensation and other body functions below the site of the injury.
Your ability to control your limbs after a spinal cord injury depends on two factors: where the injury occurred on your spinal cord and the severity of injury.
Spinal cord injuries can cause one or more of the following signs and symptoms:
- Loss of movement
- Loss of or altered sensation, including the ability to feel heat, cold and touch
- Loss of bowel or bladder control
- Exaggerated reflex activities or spasms
- Changes in sexual function, sexual sensitivity and fertility
- Pain or an intense stinging sensation caused by damage to the nerve fibers in your spinal cord
- Difficulty breathing, coughing or clearing secretions from your lungs
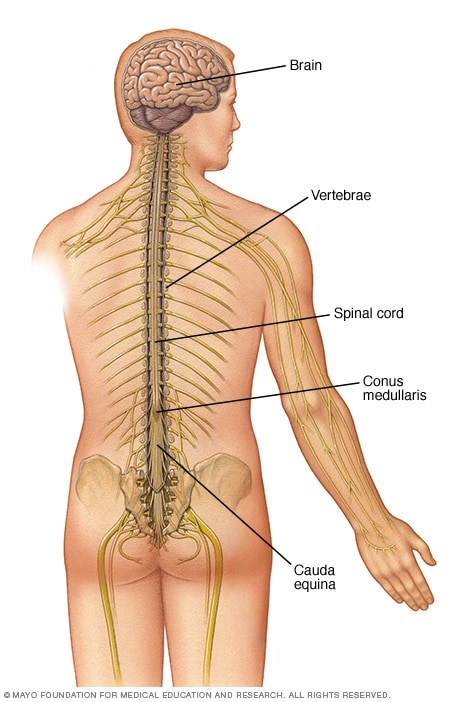
Anyone who has significant trauma to the head or neck needs immediate medical evaluation for a spinal injury.
To determine the most appropriate plan of action make an appointment today. Goals Healthcare can propose treatment options based on your specific needs.
Stroke - Pre and Post Stroke Care
A stroke occurs when the blood supply to part of your brain is interrupted or reduced, depriving brain tissue of oxygen and nutrients.
If you feel signs and symptoms of a stroke are affecting you or a loved one please consider seeking care. When possible, pay attention to the signs and symptoms and how they begin or try to remember when they originally began. The length of time they have been present or were present before your stroke occurred.
Understanding when the stroke occurred or what will trigger one can affect your treatment options.
- Trouble with speaking and understanding. You may experience confusion. You may slur your words or have difficulty understanding speech.
- Paralysis or numbness of the face, arm or leg. You may develop sudden numbness, weakness or paralysis in your face, arm or leg. This often happens just on one side of your body. Try to raise both your arms over your head at the same time. If one arm begins to fall, you may be having a stroke. Also, one side of your mouth may droop when you try to smile.
- Trouble with seeing in one or both eyes. You may suddenly have blurred or blackened vision in one or both eyes, or you may see double.
- Headache. A sudden, severe headache, which may be accompanied by vomiting, dizziness or altered consciousness, may indicate you’re having a stroke.
- Trouble with walking. You may stumble or experience sudden dizziness, loss of balance or loss of coordination.
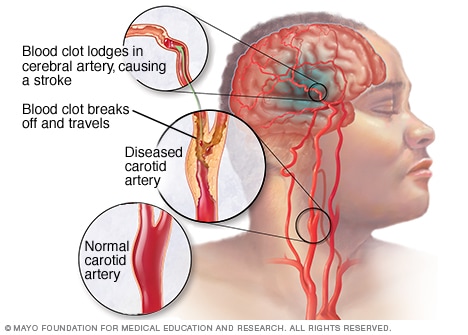
To determine the most appropriate treatment for your stroke, the type of stroke you may have and the areas of your brain affected are critical to understanding how to treat signs and symptoms. Ruling out other possible causes, such as a brain tumor or a drug reaction is also equally as important. It may take several tests to determine the cause and additional risks or treatment but Goals Healthcare will be with you throughout the entire process.
Together we will achieve progress!
Trigger Point Injections (Muscle "Knots")
A trigger point injection can help relieve myofascial pain in your neck, shoulder and arms. Trigger points are painful “knots” in your muscles that can be very sensitive.
They may form after acute trauma or by repetitive micro-trauma, leading to stress on muscle fibers. It causes the muscle fibers to be stuck in a contracted state. Sometimes you can feel these knots when you rub your muscle.
What to expect during Trigger Point Injections
- Trigger point injections commonly involve injections of local anesthetic with or without corticosteroid and/or botulinum toxin.
- During trigger point injections a thin needle attached to a syringe will be placed into the knot and rhythmically continue needling the area by repeatedly inserting and retracting the needle without completely withdrawing the needle from the muscle or your skin.
- You’ll likely feel your muscle spasm or twitch.
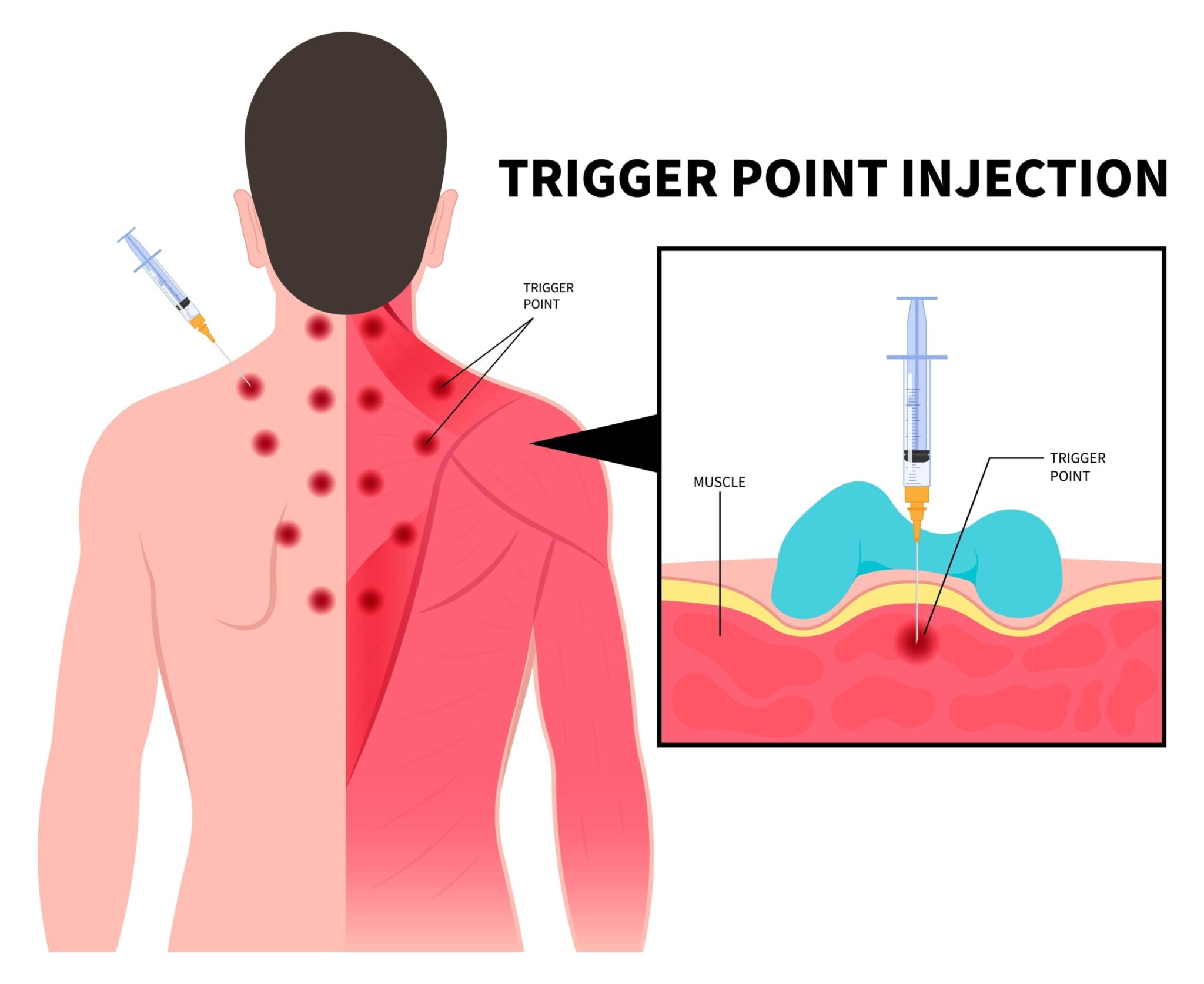
If you regularly have signs and symptoms of pain in the head, neck or shoulder area, keep a record of the pain and how you treated it.
Some insurance plans will cover a portion of or all costs associated with treatment. Make an appointment with Goals Healthcare to learn if Trigger Point Injections are right for you.
Vertigo (Dizziness)
One of the most common causes of vertigo is benign paroxysmal positional vertigo (BPPV), the sudden sensation that you’re spinning or that the inside of your head is spinning.
Benign paroxysmal positional vertigo causes brief episodes of mild to intense dizziness.
The signs and symptoms may also include
- A sense that you or your surroundings are spinning or moving (vertigo)
- A loss of balance or unsteadiness
- Nausea
- Vomiting
Benign paroxysmal positional vertigo is usually triggered by specific changes in the position of your head. This might occur when you tip your head up or down, when you lie down, or when you turn over or sit up in bed.
Book an appointment with Goals Healthcare today if you feel symptoms of vertigo are affecting your daily life. Receive a plan of action customized to your specific needs.
General Healthcare
Evaluation, Treatment or Referral
Acne
Acne is a skin condition that occurs when your hair follicles become plugged with dead skin cells.
It often causes whiteheads, blackheads or pimples, and usually appears on the face, forehead, chest, upper back and shoulders.

Acne affects people of all ages. Effective treatments are available, but acne can be persistent.
Depending on its severity Goals Healthcare has treatment options and plans customized for Your skin ready to go!
Adrenal Disease Referrals
The adrenal glands are small glands located on top of each kidney. They produce hormones that you can’t live without, including sex hormones and cortisol. Cortisol helps you respond to stress and has many other important functions.
With adrenal gland disorders, your glands make too much or not enough hormones. In Cushing’s syndrome, there’s too much cortisol, while with Addison’s disease, there is too little. Some people are born unable to make enough cortisol.
Causes of adrenal gland disorders include
- Genetic mutations
- Tumors including pheochromocytomas (A hormone-secreting tumor that can occur in the adrenal glands)
- Infections
- A problem in another gland, such as the pituitary, which helps to regulate the adrenal gland
- Certain medicines
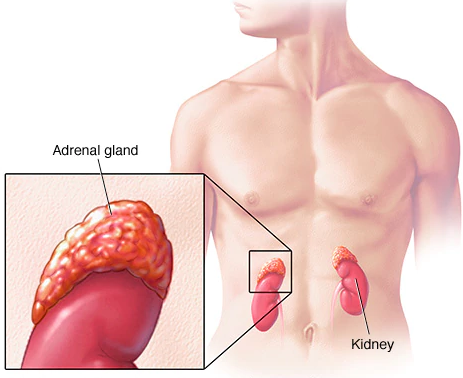
Treatment depends on which problem you have. Surgery or medicines can treat many adrenal gland disorders.
It’s important if you are experiencing any symptoms to make an appointment so we can help you diagnose the problem and refer you to the right specialist if needed.
Allergies
Allergies occur when your immune system reacts to a foreign substance such as pollen, bee venom, pet dander or a food that doesn’t cause a reaction in most people.
Your immune system produces substances known as antibodies. When you have allergies, your immune system makes antibodies that identify a particular allergen as harmful, even though it isn’t. When you come into contact with the allergen, your immune system’s reaction can inflame your skin, sinuses, airways or digestive system.
Allergy symptoms, which depend on the substance involved, can affect your airways, sinuses, nasal passages, skin, and digestive system. The severity of allergies varies from person to person and can range from minor irritation to anaphylaxis, a potentially life-threatening emergency.
While most allergies can’t be cured, treatments and diet can help relieve your allergy symptoms.

Hay fever, also called allergic rhinitis, can cause
- Sneezing
- Itching of the nose, eyes or roof of the mouth
- Runny, stuffy nose
- Watery, red or swollen eyes (conjunctivitis)

A food allergy can cause
- Tingling in the mouth
- Swelling of the lips, tongue, face or throat
- Hives
- Anaphylaxis

An insect sting allergy can cause
- A large area of swelling (edema) at the sting site
- Itching or hives all over the body
- Cough, chest tightness, wheezing or shortness of breath
- Anaphylaxis
A drug allergy can cause
- Hives
- Itchy skin
- Rash
- Facial swelling
- Wheezing
- Anaphylaxis
Atopic dermatitis, an allergic skin condition also called eczema, can cause skin to
- Itch
- Redden
- Flake or peel

Some types of allergies, including allergies to foods and insect stings, can trigger a severe reaction known as Anaphylaxis. A life-threatening medical emergency, anaphylaxis can cause you to go into shock. Signs and symptoms of anaphylaxis include
- Loss of consciousness
- A drop in blood pressure
- Severe shortness of breath
- Skin rash
- Lightheadedness
- A rapid, weak pulse
- Nausea and vomiting
If you feel you’re being impacted by allergies Goals Healthcare can help you diagnose where it’s coming from and your best plan of action to keep symptoms away.
Allergies - Sweating and Exercise Induced
Eating certain foods may cause some people to feel itchy and lightheaded soon after starting to exercise. Serious cases may even involve hives or anaphylaxis. Not eating for a couple of hours before exercising and avoiding certain foods may help prevent this problem.
Having a plan pre and post workout is essential if you are having issues getting through your exercise sessions without symptoms.

Weekly, custom, food and diet plans based on your sensitivity and allergy Goals can be provided with our telemedicine memberships.
There’s no perfect test used to confirm or rule out a food sensitivity, intolerance and allergies but together we will figure out the best plan of action built for You.
Asthma
Asthma is a condition in which your airways narrow and swell and produce extra mucus.
This can make breathing difficult and trigger coughing, wheezing and shortness of breath.
For some people, asthma is a minor nuisance. For others, it can be a major problem that interferes with daily activities and may lead to a life-threatening asthma attack.
Asthma can’t be cured, but its symptoms can be controlled.
Because asthma often changes over time, it’s important that you work with your doctor to track your signs and symptoms and adjust treatment as needed.
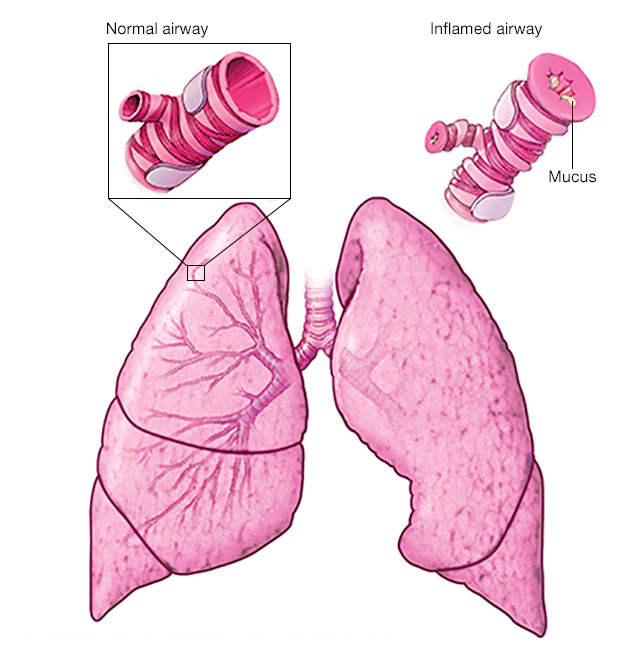
Asthma signs and symptoms include
- Shortness of breath
- Chest tightness or pain
- Trouble sleeping caused by shortness of breath, coughing or wheezing
- A whistling or wheezing sound when exhaling (wheezing is a common sign of asthma in children)
- Coughing or wheezing attacks that are worsened by a respiratory virus, such as a cold or the flu
Signs that your asthma is probably worsening include
- Asthma signs and symptoms that are more frequent and bothersome
- Increasing difficulty breathing (measurable with a peak flow meter, a device used to check how well your lungs are working)
- The need to use a quick-relief inhaler more often
For some people, asthma signs and symptoms flare up in certain situations like
- Exercise-induced asthma, which may be worse when the air is cold and dry
- Occupational asthma, triggered by workplace irritants such as chemical fumes, gases or dust
- Allergy-induced asthma, triggered by airborne substances, such as pollen, mold spores, cockroach waste or particles of skin and dried saliva shed by pets (pet dander)

If you feel asthma is affecting your daily life or if you currently have asthma and are worried about new signs and symptoms, please make an appointment with Goals Healthcare as soon as possible. Together we will breathe easier.
Autoimmune Disorders
Primary immunodeficiency disorders also called primary immune disorders or primary immunodeficiency weaken the immune system, allowing infections and other health problems to occur more easily.
Many people with primary immunodeficiency are born missing some of the body’s immune defenses, which leaves them more susceptible to germs that can cause infections.
Some forms of primary immunodeficiency are so mild they may go unnoticed for years.

Other types are severe enough that they’re discovered almost as soon as an affected baby is born.
Treatments can boost the immune system for many types of primary immunodeficiency disorders.
Most people with the condition lead relatively normal, productive lives.
Symptoms
One of the most common signs of primary immunodeficiency is an increased susceptibility to infections. You may have infections that are more frequent, longer lasting or harder to treat than are the infections of someone with a normal immune system.
You may also get infections that a person with a healthy immune system likely wouldn’t get (opportunistic infections).
Signs and symptoms differ depending on the type of primary immunodeficiency disorder, and they vary from person to person.

Signs and symptoms of primary immunodeficiency can include
- Frequent and recurrent pneumonia, bronchitis, sinus infections, ear infections, meningitis or skin infections
- Inflammation and infection of internal organs
- Blood disorders, such as low platelet counts or anemia
- Digestive problems, such as cramping, loss of appetite, nausea and diarrhea
- Delayed growth and development
- Autoimmune disorders, such as lupus, rheumatoid arthritis or type 1 diabetes
Early diagnosis and treatment of primary immune deficiencies may prevent infections that can cause long-term problems.
Causes
Many primary immunodeficiency disorders are inherited, passed down from one or both parents. Problems in the DNA, the genetic code that acts as a blueprint for producing the cells that make up the human body cause many of the immune system defects in primary immunodeficiency.

There are numerous types of primary immunodeficiency disorders.
- Rheumatoid arthritis – A chronic inflammatory disorder affecting many joints, including those in the hands and feet.
- Lupus – An inflammatory disease caused when the immune system attacks its own tissues.
- Celiac disease – An immune reaction to eating gluten, a protein found in wheat, barley, and rye.
- Sjogren’s syndrome – An immune system disorder characterized by dry eyes and dry mouth.
- Polymyalgia rheumatica – An inflammatory disorder causing muscle pain and stiffness around the shoulders and hips.
- Multiple sclerosis – A disease in which the immune system eats away at the protective covering of nerves.
- Ankylosing spondylitis – An inflammatory arthritis affecting the spine and large joints.
- Type 1 diabetes – A chronic condition in which the pancreas produces little or no insulin.
- Alopecia areata – Sudden hair loss that starts with one or more circular bald patches that may overlap.
- Vasculitis – An inflammation of the blood vessels that causes changes in the blood vessel walls.
- Temporal arteritis – An inflammation of blood vessels, called arteries, in and around the scalp.
Receive a complete insight into causes, symptoms and beneficial treatments with strategies based on Your unique situation.
Bloating (Infection or Gas)
Giardia infection is an intestinal infection marked by abdominal cramps, bloating, nausea and bouts of watery diarrhea.
Giardia infection is caused by a microscopic parasite that is found worldwide, especially in contaminated water.

Some people with giardia infection never develop signs or symptoms but still carry the parasite and can spread it to others through their stool.
For those who do get sick, signs and symptoms usually appear one to three weeks after exposure and may include
- Watery, sometimes foul-smelling diarrhea that may alternate with soft, greasy stools
- Fatigue or malaise
- Abdominal cramps and bloating
- Gas or flatulence
- Nausea
- Weight loss
Bloating from gas or gas pains can be so persistent or severe that they interfere with your ability to function well in daily life.

Gas or gas pains accompanied by other signs or symptoms may indicate a more-serious condition.
If you experience any of these additional signs or symptoms please make an appointment as soon as possible
- Bloody stools
- Change in consistency of stools
- Change in frequency of bowel movements
- Weight loss
- Constipation or diarrhea
- Persistent or recurrent nausea or vomiting
Make your appointment with Goals Healthcare if bloating symptoms are affecting your daily life. Feeling better is right around the corner.
Bloodstream Infections
Bloodstream infections (BSI) are infectious diseases defined by the presence of viable bacterial or fungal microorganisms in the bloodstream (later demonstrated by the positivity of one or more blood cultures) that elicit or have elicited an inflammatory response characterized by the alteration of clinical, laboratory and hemodynamic parameters.
BSI can be categorized in 3 main groups if occurring
- in immunologically normal hosts, with intact defenses,
- in patients with physiological condition impairing defenses, (newborns, elderly)
- in patients affected by pathological or pharmacological conditions predisposing to infections.
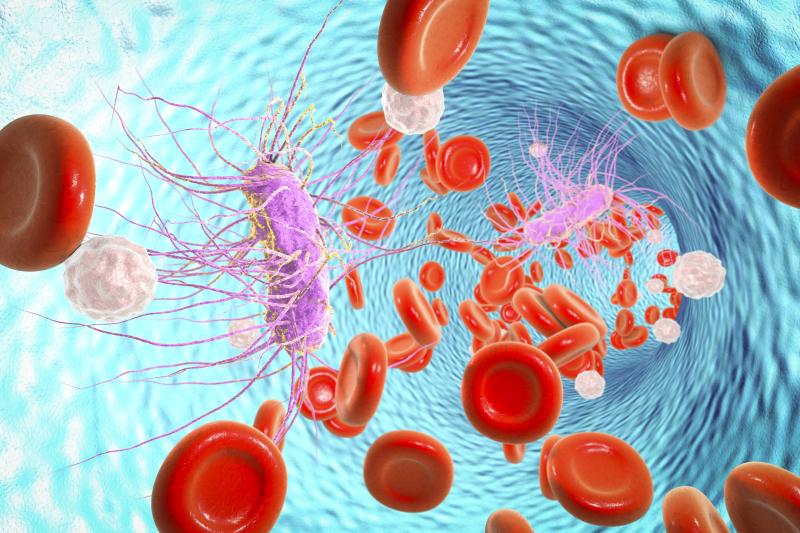
Treatments may vary. Antiviral therapy can be used in the treatment of suspected disseminated viral infections. Duration of therapy depends on several factors, including isolated pathogen, retention of catheter, or presence of complications (endocarditis, sepsis).
If you need an immediate assessment of your infection please use our telemedicine service or book your visit in office today.
Cancer Screenings
Diagnosing cancer at its earliest stages often provides the best chance for long-term success. With this in mind, we urge you to speak with us about what types of cancer screenings may be appropriate for you.
Studies show screening tests can save lives by diagnosing cancer early. For other cancers, screening tests are recommended only for people with increased risk.
By understanding your family history and gathering a full examination of your health, Dr. Levine can give you her expert medical opinion on cancer screenings, both positively and negatively.
Having personally dealt with cancer, Dr. Levine has a unique insight as a patient, loved one and now as a healthcare provider. This full all around experience with cancer allows her to connect with patients on a more personal level.
If you have any questions concerning cancer screenings or would like to schedule an assessment please make a same or next day appointment online or in-office.
Cellulitis
Cellulitis (sel-u-LIE-tis) is a common, potentially serious bacterial skin infection. The affected skin appears swollen and red and is typically painful and warm to the touch.
Cellulitis usually affects the skin on the lower legs, but it can occur in the face, arms and other areas. It occurs when a crack or break in your skin allows bacteria to enter.

Left untreated, the infection can spread to your lymph nodes and bloodstream and rapidly become life-threatening. It isn’t usually spread from person to person.
Possible signs and symptoms of cellulitis, which usually occur on one side of the body, include
- Red area of skin that tends to expand
- Swelling
- Tenderness
- Pain
- Warmth
- Fever
- Red spots
- Blisters
- Skin dimpling
It’s important to identify and treat cellulitis early because the condition can spread rapidly throughout your body. Speak with us today if you have symptoms of cellulitis. Treatment is available.
Chronic Fatigue
Chronic fatigue syndrome (CFS) is a complicated disorder characterized by extreme fatigue that can’t be explained by any underlying medical condition.
The fatigue may worsen with physical or mental activity, but doesn’t improve with rest.

This condition is also known as systemic exertion intolerance disease (SEID) or myalgic encephalomyelitis (ME). Sometimes it’s abbreviated as ME/CFS.
The cause of chronic fatigue syndrome is unknown.
There’s no single test to confirm a diagnosis of chronic fatigue syndrome. You may need a variety of medical tests to rule out other health problems that have similar symptoms.
Receive treatment options focusing on customized symptom relief while providing you the tools to reach your personal Goals.
Chronic Obstructive Pulmonary Disease (COPD)
is a chronic inflammatory lung disease that causes obstructed airflow from the lungs.
Symptoms include breathing difficulty, cough, mucus (sputum) production and wheezing.
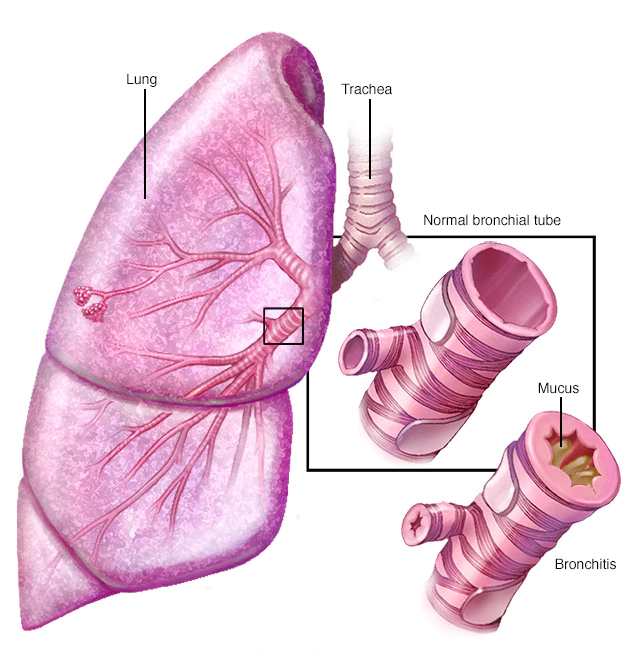
It’s caused by long-term exposure to irritating gases or particulate matter, most often from cigarette smoke. Your lungs rely on the natural elasticity of the bronchial tubes and air sacs to force air out of your body. COPD causes them to lose their elasticity and over expand, which leaves some air trapped in your lungs when you exhale.
People with COPD are at increased risk of developing heart disease, lung cancer and a variety of other conditions.
Emphysema and chronic bronchitis are the two most common conditions that contribute to COPD.
Chronic bronchitis is inflammation of the lining of the bronchial tubes, which carry air to and from the air sacs (alveoli) of the lungs. It’s characterized by daily cough and mucus (sputum) production.
Emphysema is a condition in which the alveoli at the end of the smallest air passages (bronchioles) of the lungs are destroyed as a result of damaging exposure to cigarette smoke and other irritating gases and particulate matter.
Symptoms of COPD may include
- Shortness of breath, especially during physical activities
- Wheezing
- Chest tightness
- Having to clear your throat first thing in the morning, due to excess mucus in your lungs
- A chronic cough that may produce mucus (sputum) that may be clear, white, yellow or greenish
- Blueness of the lips or fingernail beds (cyanosis)
- Frequent respiratory infections
- Lack of energy
- Unintended weight loss (in later stages)
- Swelling in ankles, feet or legs
People with COPD are also likely to experience episodes called exacerbations, during which their symptoms become worse than usual day-to-day variation and persist for at least several days.
Alpha-1-antitrypsin deficiency
In about 1 percent of people with COPD, the disease results from a genetic disorder that causes low levels of a protein called alpha-1-antitrypsin.
Alpha-1-antitrypsin (AAt) is made in the liver and secreted into the bloodstream to help protect the lungs.
Alpha-1-antitrypsin deficiency can affect the liver as well as the lungs.
Complications of COPD include
- Respiratory infections. People with COPD are more likely to catch colds, the flu and pneumonia. Any respiratory infection can make it much more difficult to breathe and could cause further damage to lung tissue. An annual flu vaccination and regular vaccination against pneumococcal pneumonia can prevent some infections.
- Heart problems. For reasons that aren’t fully understood, COPD can increase your risk of heart disease, including heart attack. Quitting smoking may reduce this risk.
- Lung cancer. People with COPD have a higher risk of developing lung cancer. Quitting smoking may reduce this risk.
- High blood pressure in lung arteries. COPD may cause high blood pressure in the arteries that bring blood to your lungs (pulmonary hypertension).
- Depression. Difficulty breathing can keep you from doing activities that you enjoy. And dealing with serious illness can contribute to development of depression. Talk to your doctor if you feel sad or helpless or think that you may be experiencing depression.
COPD is treatable. We will provide the plan necessary for you to properly manage your symptoms while improving your quality of life. Most people with COPD can achieve good symptom control and quality of life, as well as reduced risk of other associated conditions.
Common Cold
The common cold is a viral infection of your nose and throat (upper respiratory tract).
Most people recover from a common cold in a week or 10 days. Symptoms might last longer in people who smoke or those with a weaker immune system or chronic condition and older adults.
Healthy adults can expect to have two or three colds annually.
You may experience
- Fever greater than 101.3 F (38.5 C)
- Fever lasting five days or more or returning after a fever-free period
- Shortness of breath
- Wheezing
- Severe sore throat, headache or sinus pain

Goals Healthcare can help you get back to full speed when the common cold just will not go away.
Diabetes Evaluation and Management
Diabetes mellitus refers to a group of diseases that affect how your body uses blood sugar (glucose). Glucose is vital to your health because it’s an important source of energy for the cells that make up your muscles and tissues. Glucose is also your brain’s main source of fuel.
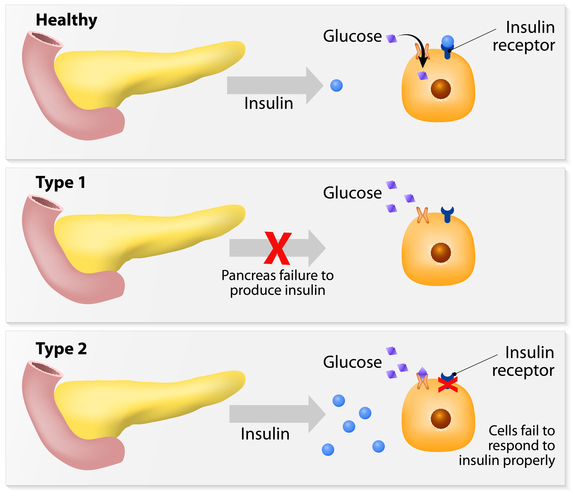
The underlying cause of diabetes varies by type. But, no matter what type of diabetes you have, it can lead to excess sugar in your blood. Too much sugar in your blood can lead to serious health problems.
Chronic diabetes conditions include type 1 diabetes and type 2 diabetes.
Potentially reversible diabetes conditions include prediabetes when your blood sugar levels are higher than normal, but not high enough to be classified as diabetes.

Diabetes symptoms vary depending on how much your blood sugar is elevated. Some people, especially those with prediabetes or type 2 diabetes, may not experience symptoms initially.
In type 1 diabetes, symptoms tend to come on quickly and be more severe.
Some of the signs and symptoms of type 1 and type 2 diabetes are
- Increased thirst
- Frequent urination
- Extreme hunger
- Unexplained weight loss
- Presence of ketones in the urine (ketones are a byproduct of the breakdown of muscle and fat that happens when there’s not enough available insulin)
- Fatigue
- Irritability
- Blurred vision
- Slow-healing sores
- Frequent infections, such as gums or skin infections and vaginal infections
Causes of type 1 diabetes
The exact cause of type 1 diabetes is unknown. What is known is that your immune system which normally fights harmful bacteria or viruses attacks and destroys your insulin-producing cells in the pancreas. This leaves you with little or no insulin. Instead of being transported into your cells, sugar builds up in your bloodstream.
Type 1 is thought to be caused by a combination of genetic susceptibility and environmental factors, though exactly what those factors are is still unclear. Weight is not believed to be a factor in type 1 diabetes.

Causes of prediabetes and type 2 diabetes
In prediabetes which can lead to type 2 diabetes and in type 2 diabetes, your cells become resistant to the action of insulin, and your pancreas is unable to make enough insulin to overcome this resistance. Instead of moving into your cells where it’s needed for energy, sugar builds up in your bloodstream.
Exactly why this happens is uncertain, although it’s believed that genetic and environmental factors play a role in the development of type 2 diabetes too. Being overweight is strongly linked to the development of type 2 diabetes, but not everyone with type 2 is overweight.
Causes of gestational diabetes
During pregnancy, the placenta produces hormones to sustain your pregnancy. These hormones make your cells more resistant to insulin.
Normally, your pancreas responds by producing enough extra insulin to overcome this resistance. But sometimes your pancreas can’t keep up. When this happens, too little glucose gets into your cells and too much stays in your blood, resulting in gestational diabetes.
Although the exact cause of type 1 diabetes is unknown, factors that may signal an increased risk include
- Family history. Your risk increases if a parent or sibling has type 1 diabetes.
- Environmental factors. Circumstances such as exposure to a viral illness likely play some role in type 1 diabetes.
- The presence of damaging immune system cells (autoantibodies). Sometimes family members of people with type 1 diabetes are tested for the presence of diabetes autoantibodies. If you have these autoantibodies, you have an increased risk of developing type 1 diabetes. But not everyone who has these autoantibodies develops diabetes.
- Geography. Certain countries, such as Finland and Sweden, have higher rates of type 1 diabetes.
It’s clear that certain factors increase the risk including
- Weight. The more fatty tissue you have, the more resistant your cells become to insulin.
- Inactivity. The less active you are, the greater your risk. Physical activity helps you control your weight, uses up glucose as energy and makes your cells more sensitive to insulin.
- Family history. Your risk increases if a parent or sibling has type 2 diabetes.
- Race. Although it’s unclear why, people of certain races — including black people, Hispanics, American Indians and Asian-Americans — are at higher risk.
- Age. Your risk increases as you get older. This may be because you tend to exercise less, lose muscle mass and gain weight as you age. But type 2 diabetes is also increasing among children, adolescents and younger adults.
- Gestational diabetes. If you developed gestational diabetes when you were pregnant, your risk of developing prediabetes and type 2 diabetes later increases. If you gave birth to a baby weighing more than 9 pounds (4 kilograms), you’re also at risk of type 2 diabetes.
- Polycystic ovary syndrome. For women, having polycystic ovary syndrome — a common condition characterized by irregular menstrual periods, excess hair growth and obesity — increases the risk of diabetes.
- High blood pressure. Having blood pressure over 140/90 millimeters of mercury (mm Hg) is linked to an increased risk of type 2 diabetes.
- Abnormal cholesterol and triglyceride levels. If you have low levels of high-density lipoprotein (HDL), or “good,” cholesterol, your risk of type 2 diabetes is higher. Triglycerides are another type of fat carried in the blood. People with high levels of triglycerides have an increased risk of type 2 diabetes. Your doctor can let you know what your cholesterol and triglyceride levels are.

Each person is unique in their own way. Goals Healthcare works with you to find the right course of treatment designed specifically for You.
Diabetic Neuropathy
Diabetic neuropathy is a type of nerve damage that can occur if you have diabetes. High blood sugar (glucose) can injure nerves throughout your body. Diabetic neuropathy most often damages nerves in your legs and feet.
Depending on the affected nerves, symptoms of diabetic neuropathy can range from pain and numbness in your legs and feet to problems with your digestive system, urinary tract, blood vessels and heart.
Some people have mild symptoms. But for others, diabetic neuropathy can be quite painful and disabling.
Peripheral neuropathy is the most common type of diabetic neuropathy. It affects the feet and legs first, followed by the hands and arms.
Signs and symptoms of peripheral neuropathy are often worse at night, and may include
- Numbness or reduced ability to feel pain or temperature changes
- Tingling or burning sensation
- Sharp pains or cramps
- Increased sensitivity to touch — for some people, even the weight of a bedsheet can be painful
- Muscle weakness
- Loss of reflexes, especially in the ankle
- Loss of balance and coordination
- Serious foot problems, such as ulcers, infections, and bone and joint pain
If you have diabetes and need help dealing with symptoms like neuropathy, Goals Healthcare will present a plan of action for treatment and a referral to a Neuromuscular specialist if needed.
Diabetic Swelling (Gangrene)
Gangrene refers to the death of body tissue due to either a lack of blood flow or a serious bacterial infection.
Gangrene commonly affects the extremities, including your toes, fingers and limbs, but it can also occur in your muscles and internal organs.

Your chances of developing gangrene are higher if you have an underlying condition that can damage your blood vessels and affect blood flow, such as diabetes or hardened arteries (atherosclerosis).
If you have a type of gangrene that affects tissues beneath the surface of your skin, such as gas gangrene or internal gangrene, you may notice that
- The affected tissue is swollen and very painful
- You’re running a low-grade fever and generally feel unwell
When gangrene affects your skin, signs and symptoms may also include
- Skin discoloration ranging from pale to blue, purple, black, bronze or red, depending on the type of gangrene you have
- Swelling or the formation of blisters filled with fluid on the skin
- A clear line between healthy and damaged skin
- Sudden, severe pain followed by a feeling of numbness
- A foul-smelling discharge leaking from a sore
- Thin, shiny skin, or skin without hair
- Skin that feels cool or cold to the touch
Tissue that has been damaged by gangrene can not be saved, but steps can be taken to prevent gangrene from spreading. Depending on the severity of your gangrene, we will present to you the best treatment options and a plan of action moving forward.
Drop Foot
Foot drop, sometimes called drop foot, is a general term for difficulty lifting the front part of the foot. Foot drop isn’t a disease. Rather, foot drop is a sign of an underlying neurological, muscular or anatomical problem.
If you have foot drop, the front of your foot might drag on the ground when you walk.
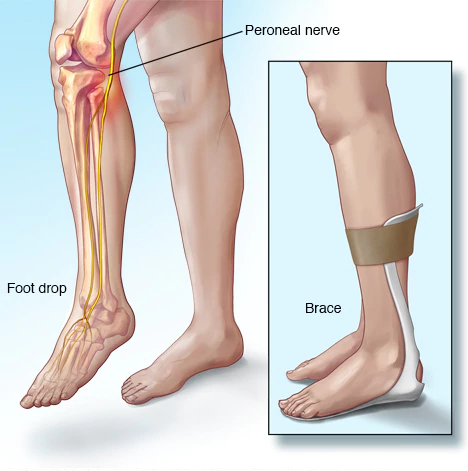
Sometimes foot drop is temporary, but it can be permanent. If you have foot drop, you might need to wear a brace on your ankle and foot to hold your foot in a normal position.
Foot drop makes it difficult to lift the front part of your foot, so it might drag on the floor when you walk. This can cause you to raise your thigh when you walk, as though climbing stairs (steppage gait), to help your foot clear the floor.
This unusual gait might cause you to slap your foot down onto the floor with each step. In some cases, the skin on the top of your foot and toes feels numb.
During your physical exam Dr. Levine will try and determine the cause of your drop foot and if necessary, refer you for a nerve conduction study, conducted by a Neurologist and/or Neuromuscular Specialist.
These tests are very useful in determining the location of the damage along the affected nerve.
Dry Mouth (Excessive)
Dry mouth, or xerostomia (zeer-o-STOE-me-uh), refers to a condition in which the salivary glands in your mouth don’t make enough saliva to keep your mouth wet.
Dry mouth is often due to the side effect of certain medications or aging issues or as a result of radiation therapy for cancer.
Less often, dry mouth may be caused by a condition that directly affects the salivary glands.
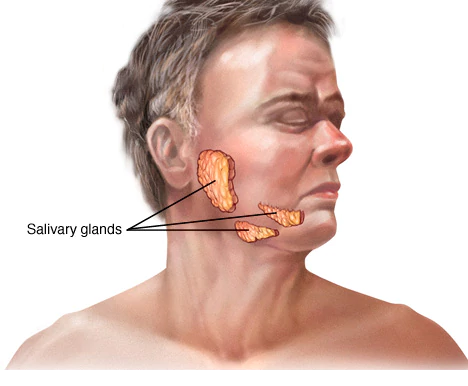
Decreased saliva and dry mouth can range from being merely a nuisance to something that has a major impact on your general health and the health of your teeth and gums, as well as your appetite and enjoyment of food.
Treatment for dry mouth depends on the cause. Come in for your exam and receive treatment options based on your diagnosis.
Dry, Itchy and Scaly Skin (Excessive)
Itchy skin is an uncomfortable, irritating sensation that makes you want to scratch. Also known as pruritus (proo-RIE-tus), itchy skin is usually caused by dry skin.
It’s common in older adults, as skin tends to become drier with age.

Depending on the cause of your itchy skin, it may appear normal. Or it may be red or rough or have bumps or blisters. Repeated scratching can cause raised, thickened areas of skin that may bleed or become infected.
Long-term relief requires identifying and treating the cause of your dry and itchy skin.
Dry and itchy skin isn’t usually serious, but it can be uncomfortable and unsightly.
Serious dry and itchy skin conditions, an inherited group of disorders called ichthyosis, can sometimes be disfiguring and upsetting. Fortunately, most dry and itchy skin can be at least partially controlled.

If you experience any of the below symptoms come in for an assessment and Goals can help start the process of making you feel more comfortable in your own skin.
- Your skin doesn’t improve in spite of your best efforts
- Dry skin is accompanied by redness
- Dryness and itching interfere with sleeping
- You have open sores or infections from scratching
- You have large areas of scaling or peeling skin
For an immediate examination please use our telemedicine service online or make your same-day appointment now.
Ear Ache (Infection)
An ear infection (acute otitis media) is most often a bacterial or viral infection that affects the middle ear, the air-filled space behind the eardrum that contains the tiny vibrating bones of the ear.
Ear infections frequently are painful because of inflammation and buildup of fluids in the middle ear.
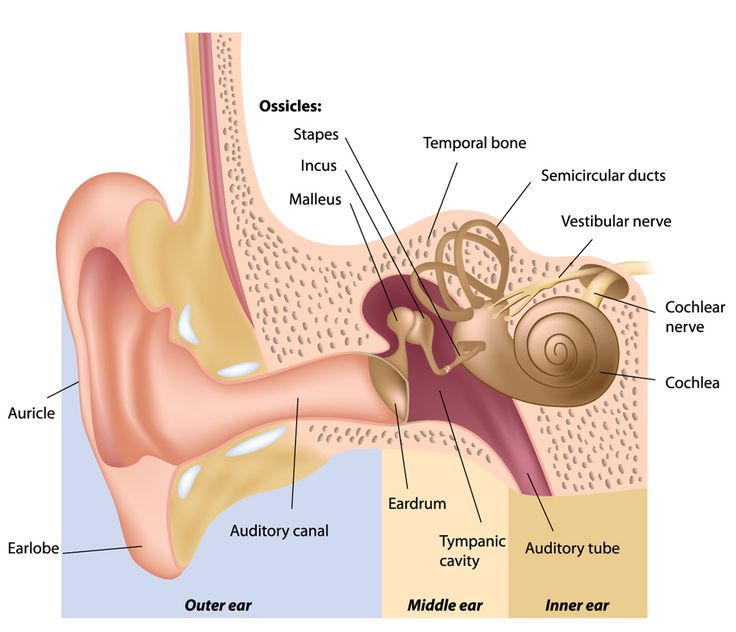
Because ear infections often clear up on their own, treatment may begin with managing pain and monitoring the problem.
Long-term problems related to ear infections like persistent fluids in the middle ear, persistent infections or frequent infections can cause hearing problems and other serious complications.
Common signs and symptoms in include
- Ear pain
- Drainage of fluid from the ear
- Diminished hearing
If your signs and symptoms last for more than 2 days contact Goals Healthcare for a complete ear assessment and treatments to quickly make the infection disappear.
Ear Wax Removal - Cerumen
Let’s face it New York and daily life in general can be dirty and building ear wax is a natural defense mechanism for your ears.
Earwax blockage occurs when earwax (cerumen) accumulates in your ear or becomes too hard to wash away naturally.
Earwax is a helpful and natural part of your body’s defenses. It cleans, lubricates and protects your ear canal by trapping dirt and slowing the growth of bacteria.
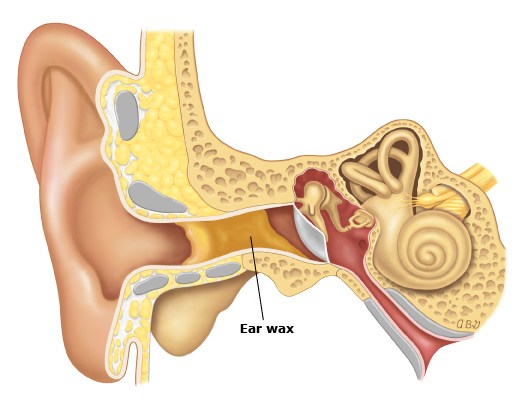
If earwax blockage becomes a problem Dr. Levine can take simple steps to remove the wax safely.
Signs and symptoms of earwax blockage may include
- Earache
- Feeling of fullness in the affected ear
- Ringing or noises in the ear (tinnitus)
- Decreased hearing in the affected ear
- Dizziness
- Cough
If signs and symptoms are giving you issues come in for an appointment today.
Eczema (Dermatitis)
or Dermatitis is a general term that describes an inflammation of the skin.
Dermatitis can have many causes and occurs in many forms. It usually involves an itchy rash on swollen, reddened skin. Skin affected by dermatitis may blister, ooze, develop a crust or flake off.

Examples of dermatitis include atopic dermatitis Eczema, dandruff and rashes caused by contact with any of a number of substances, such as poison ivy, soaps and jewelry with nickel in it.
Dermatitis is a common condition that’s not contagious, but it can make you feel uncomfortable and self-conscious. A combination of self-care steps and medications can help you treat dermatitis.
Each type of dermatitis may look a little different and tends to occur on different parts of your body.
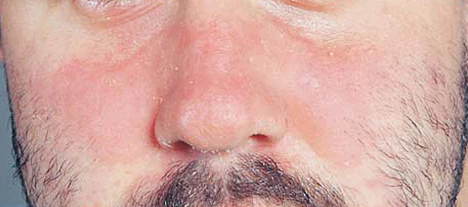
The most common types of dermatitis include
- Atopic dermatitis (Eczema). Usually beginning in infancy, this red, itchy rash most commonly occurs where the skin flexes — inside the elbows, behind the knees and the front of the neck. When scratched, the rash can leak fluid and crust over. People with atopic dermatitis may experience improvement and then flare-ups.
- Contact dermatitis. This rash occurs on areas of the body that have come into contact with substances that either irritate the skin or cause an allergic reaction, such as poison ivy, soap and essential oils. The red rash may burn, sting or itch. Blisters may develop.
- Seborrheic dermatitis. This condition causes scaly patches, red skin and stubborn dandruff. It usually affects oily areas of the body, such as the face, upper chest and back. It can be a long-term condition with periods of remission and flare-ups. In infants, this disorder is known as cradle cap.

A number of health conditions, allergies, genetic factors and irritants can cause different types of dermatitis
- Atopic dermatitis (Eczema). This form of dermatitis is likely related to a mix of factors, including dry skin, a gene variation, an immune system dysfunction, bacteria on the skin and environmental conditions.
- Contact dermatitis. This condition results from direct contact with one of many irritants or allergens such as poison ivy, jewelry containing nickel, cleaning products, perfumes, cosmetics, and even the preservatives in many creams and lotions.
- Seborrheic dermatitis. This condition may be caused by a yeast (fungus) that is in the oil secretion on the skin. People with seborrheic dermatitis may notice their condition tends to come and go depending on the season.
We will break down for you the type of dermatitis you have, and your plan of action to contain the symptoms, redness and eliminate scaly skin.
Make your appointment today for an in-office assessment or get started by using our telemedicine service online.
Fibromyalgia
Fibromyalgia is a disorder characterized by widespread musculoskeletal pain accompanied by fatigue, sleep, memory and mood issues.
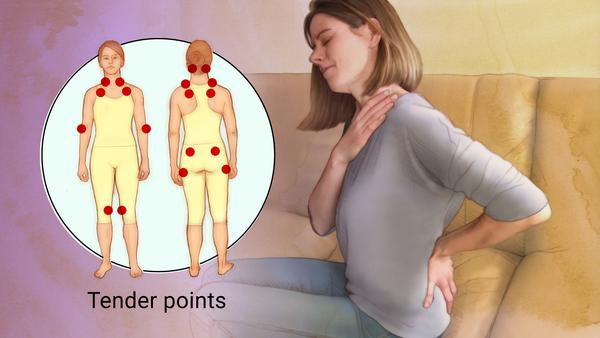
Symptoms sometimes begin after a physical trauma, surgery, infection or significant psychological stress. In other cases, symptoms gradually accumulate over time with no single triggering event.
Many people who have fibromyalgia also have tension headaches, temporomandibular joint (TMJ) disorders, irritable bowel syndrome, anxiety and depression.
While there is no cure for fibromyalgia, a variety of medications and treatments can help control symptoms. Make an appointment today if you’re tired of fibromyalgia affecting your life.
Flu (Influenza)
The Flu is a common viral infection that can be deadly, especially in high-risk groups.
Influenza is a viral infection that attacks your respiratory system, your nose, throat and lungs.
Influenza, commonly called the flu, is not the same as stomach “flu” viruses that cause diarrhea and vomiting.
For most people, influenza resolves on its own. But sometimes, influenza and its complications can be very serious.

People at higher risk of developing flu complications include
- Adults older than 65
- Pregnant women and women up to two weeks postpartum
- People with weakened immune systems
- People who have chronic illnesses, such as asthma, heart disease, kidney disease and diabetes
- People who are very obese, with a body mass index (BMI) of 40 or higher

Common signs and symptoms of the flu include
- Fever over 100.4 F (38 C)
- Aching muscles, especially in your back, arms and legs
- Chills and sweats
- Headache
- Dry, persistent cough
- Fatigue and weakness
- Nasal congestion
- Sore throat
The bottom line is no one has time for the flu. Goals Healthcare can help you get back to full speed when the common flu just will not go away fast enough.
Flu (Stomach)
Stomach flu (viral gastroenteritis) is an intestinal infection marked by watery diarrhea, abdominal cramps, nausea or vomiting, and sometimes fever.
The most common way to develop viral gastroenteritis, often called stomach flu, is through contact with an infected person or by ingesting contaminated food or water.
If you’re otherwise healthy, you’ll likely recover without complications. But for older adults and people with compromised immune systems, viral gastroenteritis can be very serious.

Although it’s commonly called stomach flu, gastroenteritis isn’t the same as influenza. Real flu (influenza) affects only your respiratory system — your nose, throat and lungs.
Gastroenteritis, on the other hand, attacks your intestines, causing signs and symptoms, such as
- Watery, usually nonbloody diarrhea – bloody diarrhea usually means you have a different, more severe infection
- Abdominal cramps and pain
- Nausea, vomiting or both
- Occasional muscle aches or headache
- Low-grade fever
Food Intolerance and Sensitivity
While bothersome, food intolerance is a less serious condition than a food allergy and does not involve the immune system.

A careful exam can often identify or exclude other medical problems.
- A skin test test can determine your reaction to a particular food. In this test, a small amount of the suspected food is placed on the skin of your forearm or back.
- If you’re allergic to a particular substance being tested, you develop a raised bump or reaction. Keep in mind, a positive reaction to this test alone isn’t enough to confirm a food allergy.
- A blood test can measure your immune system’s response to particular foods by measuring the allergy-related antibody known as immunoglobulin E (IgE). For this test, a blood sample is sent to a laboratory, where different foods can be tested.
Weekly, custom, food and diet plans based on your sensitivity and allergy Goals can be provided with our telemedicine memberships.

There’s no perfect test used to confirm or rule out a food sensitivity, intolerance and allergies but together we will figure out the best plan of action for You.
Genetic Counseling
Understanding Your Genetics – lifestyle habits, family health and history can give you a “leg up” on your overall health.
Although genetics do not tell our entire story, we are learning they are some of the key factors in creating customized prevention strategies and treatments.

Make your appointment with Goals Healthcare today to learn more about your genetics and how they play an important role in your health.
Gout
is a common and complex form of arthritis that can affect anyone. Gout occurs when urate crystals accumulate in your joint, causing the inflammation and intense pain of a gout attack. Urate crystals can form when you have high levels of uric acid in your blood.
It’s characterized by sudden, severe attacks of pain, swelling, redness and tenderness in the joints, often the joint at the base of the big toe, but it can occur in any joint. An attack of gout can occur suddenly, often waking you up in the middle of the night with the sensation that your big toe is on fire. The affected joint is hot, swollen and so tender that even the weight of the sheet on it may seem intolerable. Other commonly affected joints include the ankles, knees, elbows, wrists and fingers.

Normally, uric acid dissolves in your blood and passes through your kidneys into your urine. But sometimes either your body produces too much uric acid or your kidneys excrete too little uric acid.
Gout symptoms may come and go, but there are ways to manage symptoms and prevent flares. Gout that goes untreated can lead to worsening pain and joint damage.
Factors that increase the uric acid level in your body include
- Eating a diet rich in meat and seafood
- Drinking beverages sweetened with fruit sugar (fructose) increase levels of uric acid, which increase your risk of gout.
- Alcohol consumption, especially of beer, also increases the risk of gout.
- Obesity. If you’re overweight, your body produces more uric acid and your kidneys have a more difficult time eliminating uric acid.
- Medical conditions such as untreated high blood pressure and chronic conditions such as diabetes, metabolic syndrome, and heart and kidney diseases.
- Certain medications
- Family history of gout
- Gout occurs more often in men, primarily because women tend to have lower uric acid levels. After menopause, however, women’s uric acid levels approach those of men.
- Men are also more likely to develop gout earlier usually between the ages of 30 and 50 whereas women generally develop signs and symptoms after menopause.
People with Untreated Gout can develop more-severe conditions, such as
- Deposits of urate crystals to form under the skin in nodules called tophi (TOE-fie).
- Tophi can develop in several areas such as your fingers, hands, feet, elbows or Achilles tendons along the backs of your ankles.
- Urate crystals may collect in the urinary tract of people with untreated gout causing kidney stones.
Make your appointment with Goals Healthcare today and together we will Gout (get) this under control.
Heart Attack and Heart Disease Risk Evaluation
The statistics for heart disease and heart attacks are extremely serious.
- About 610,000 people die of heart disease in the United States every year. That’s 1 in every 4 deaths.
- Heart disease is the leading cause of death for both men and women.
- Coronary heart disease is the most common type of heart disease, killing over 370,000 people annually.
- Every year about 735,000 Americans have a heart attack. Of these, 525,000 are a first heart attack and 210,000 happen in people who have already had a heart attack.
Heart disease describes a range of conditions that affect your heart. Diseases under the heart disease umbrella include
- blood vessel diseases, such as coronary artery disease
- heart rhythm problems (arrhythmias)
- heart defects you’re born with (congenital heart defects), among others
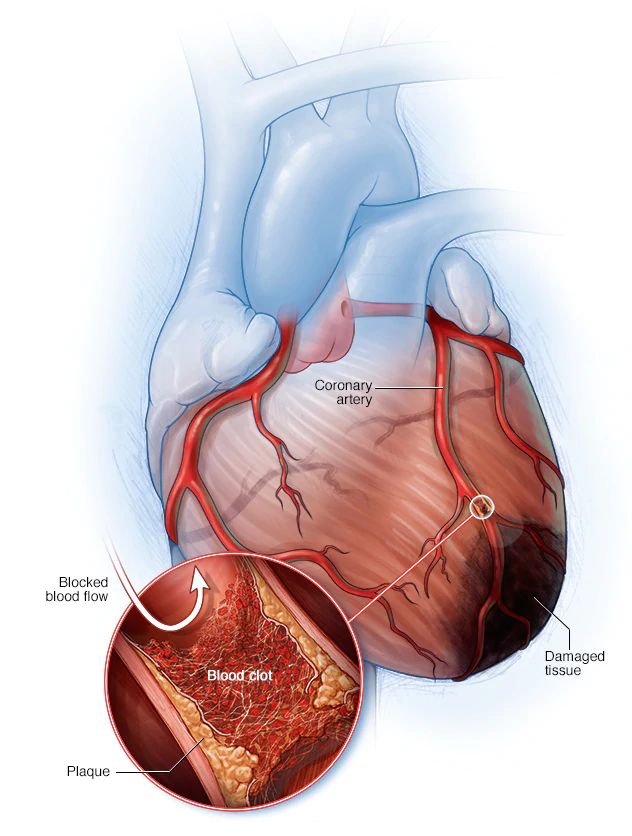
The term “heart disease” is often used interchangeably with the term “cardiovascular disease.” Cardiovascular disease generally refers to conditions that involve narrowed or blocked blood vessels that can lead to a heart attack, chest pain (angina) or stroke.
Other heart conditions, such as those that affect your heart’s muscle, valves or rhythm, also are considered forms of heart disease.
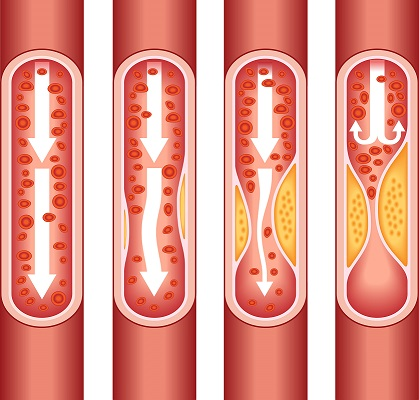
Common heart attack signs and symptoms can include
- Pressure, tightness, pain, or a squeezing or aching sensation in your chest or arms that may spread to your neck, jaw or back
- Nausea, indigestion, heartburn or abdominal pain
- Shortness of breath
- Cold sweat
- Fatigue
- Lightheadedness or sudden dizziness
Symptoms of heart disease can include
- Chest pain, chest tightness, chest pressure and chest discomfort (angina)
- Shortness of breath
- Pain, numbness, weakness or coldness in your legs or arms if the blood vessels in those parts of your body are narrowed
- Pain in the neck, jaw, throat, upper abdomen or back
It’s important that if you have a family history of heart disease, heart attacks or experiencing signs and symptoms, early care is crucial. Goals Healthcare can help you fight off symptoms while improving your heart health.
HIV Testing and Management
HIV Testing and Management – Our HIV Testing and Management with Primary Care regimen may involve multiple long-term therapies to help achieve a reduction in your viral load to the point that it’s undetectable.
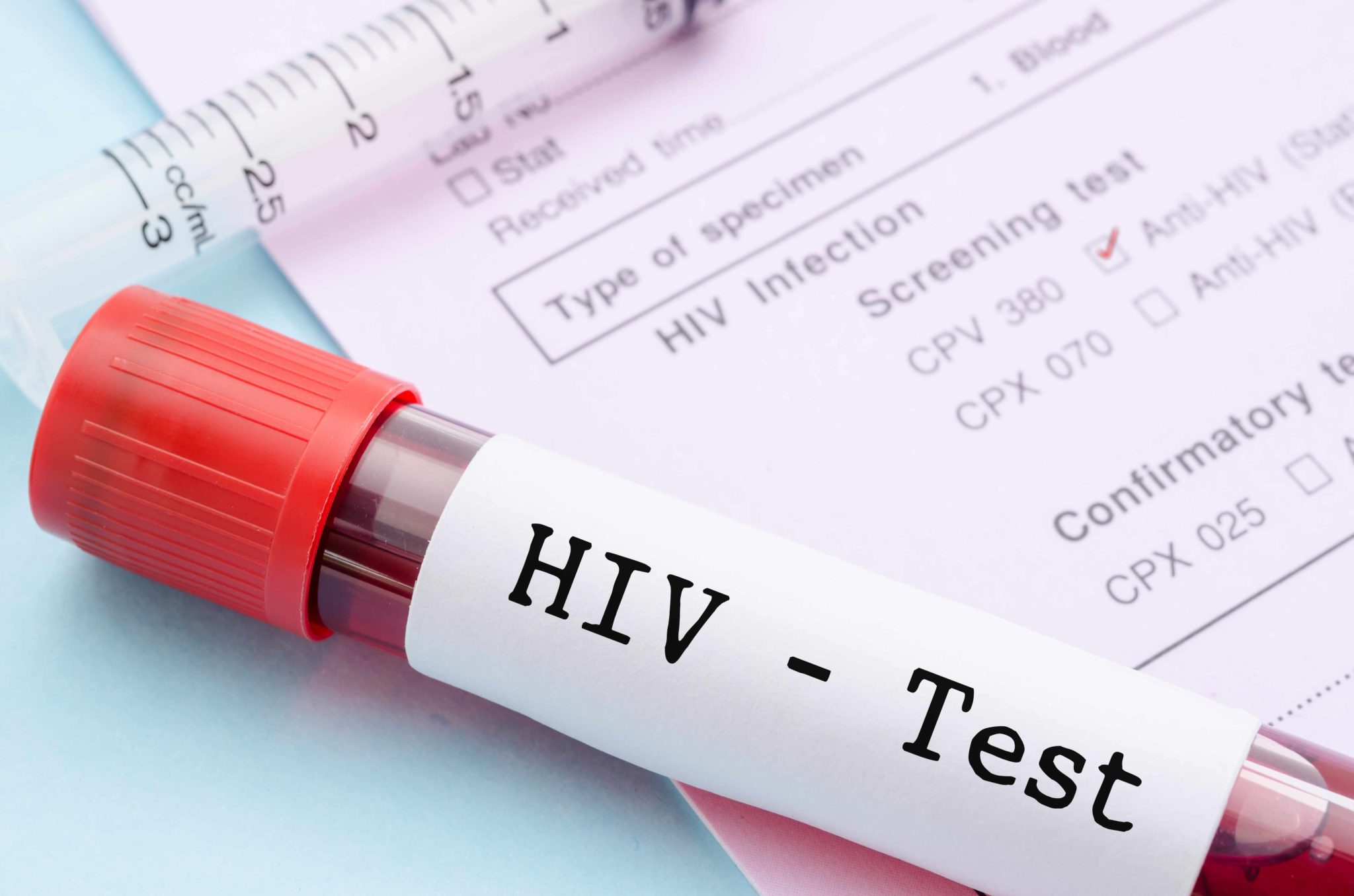
HIV treatment (antiretroviral therapy) can help you stay healthy for many years and prevent you from transmitting HIV to others. Treatment suppresses the amount of HIV in your body fluids to the point where standard tests are unable to detect any HIV, or can only find a tiny trace. This is known as “having an undetectable viral load” or “being undetectable”.
Having an undetectable viral load does not mean your HIV is gone. If you stopped treatment, your viral load would rise and become detectable again. Being undetectable does mean that you cannot pass on HIV during sex. This is what is meant by the slogan ‘Undetectable = Untransmittable’ (‘U=U’).
Book Your Visit to Get Tested or Started on Your Treatment Plan. Our Team is Ready to Support Your Health Journey.
We’re in this Together.
Hormone Balancing
Hormone and testosterone therapy comes in many forms, such as creams, gels, patches or pills. A variety of factors will dictate whether hormones and testosterone therapy can be beneficial for you.
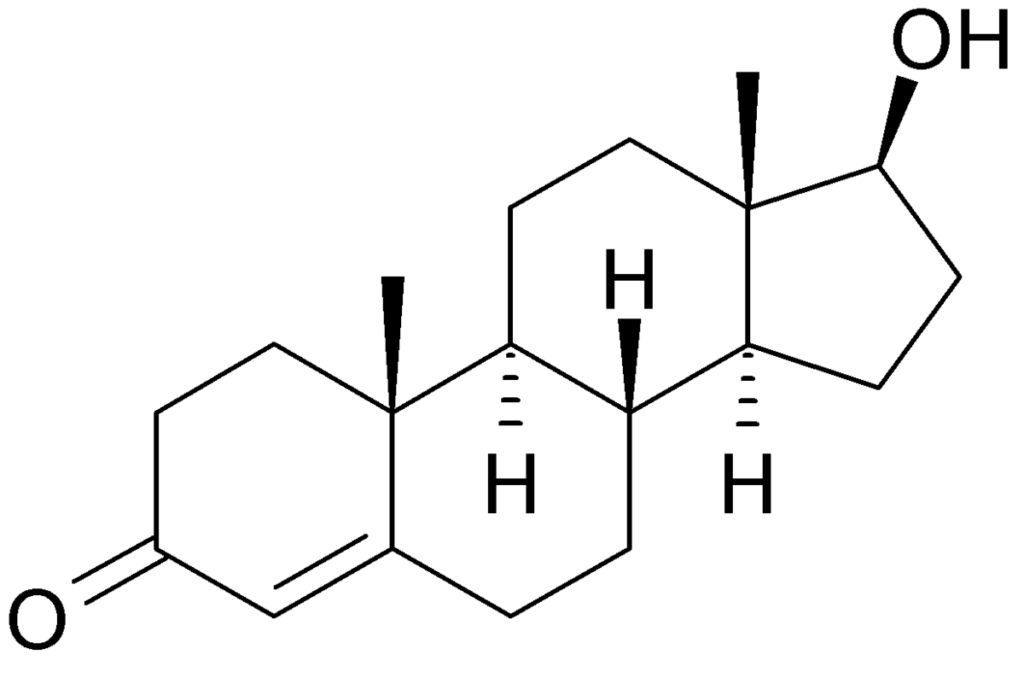
Testosterone therapy might be appropriate if
- You have reduced sex drive, depression and fatigue after surgically induced menopause, and estrogen therapy hasn’t relieved your symptoms
- You are postmenopausal, taking estrogen therapy and have a decreased sex drive with no other identifiable causes
- You mentally and physically do not feel like your adequate self

Learn if hormone and testosterone therapy is a good treatment option for you. Together we will find your best course of action.
Hospital Acquired Infections
Hospital acquired infections are caused by viral, bacterial, and fungal pathogens; the most common types are bloodstream infection (BSI), pneumonia (eg, ventilator-associated pneumonia [VAP]), urinary tract infection (UTI), and surgical site infection (SSI).

Treatments may vary. Antiviral therapy can be used in the treatment of suspected disseminated viral infections. Duration of therapy depends on several factors, including isolated pathogen, retention of catheter, or presence of complications (endocarditis, sepsis).
If you need an immediate assessment of your infection please use our telemedicine service or book your visit in office today.
Irritable Bowel Syndrome (IBS)
is a common disorder that affects the large intestine. People may experience cramping, abdominal pain, bloating, gas, and diarrhea or constipation, or both.
Most people with IBS experience times when the signs and symptoms are worse and times when they improve or even disappear completely. IBS is a chronic condition that you’ll need to manage long term.

Only a small number of people with IBS have severe signs and symptoms. Some people can control their symptoms by managing diet, lifestyle and stress. More-severe symptoms can be treated with medication and counseling.
IBS doesn’t cause changes in bowel tissue or increase your risk of colorectal cancer.
Although the signs and symptoms of IBS vary. The most common include
- Abdominal pain, cramping or bloating that is typically relieved or partially relieved by passing a bowel movement
- Excess gas
- Diarrhea or constipation — sometimes alternating bouts of diarrhea and constipation
- Mucus in the stool
A persistent change in bowel habits or other signs or symptoms of IBS that may indicate a more serious condition, such as colon cancer include
- Weight loss
- Diarrhea at night
- Rectal bleeding
- Iron deficiency anemia
- Unexplained vomiting
- Difficulty swallowing
- Persistent pain that isn’t relieved by passing gas or a bowel movement
The “bottom” line is… No one has time for IBS.
Schedule an appointment if IBS is affecting your life and you would like to discuss ways to control it.
Kidney Stones
(renal lithiasis, nephrolithiasis) are hard deposits made of minerals and salts that form inside your kidneys.
Kidney stones have many causes and can affect any part of your urinary tract from your kidneys to your bladder. Often, stones form when the urine becomes concentrated, allowing minerals to crystallize and stick together.
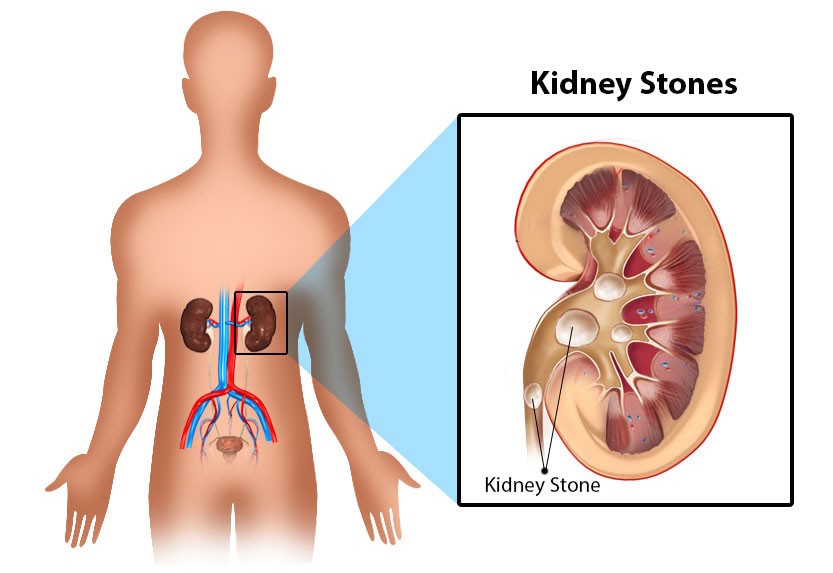
Passing kidney stones can be quite painful, but the stones usually cause no permanent damage if they’re recognized in a timely fashion.
Depending on your situation, you may need nothing more than to manage the pain and drink lots of water to pass a kidney stone. In other instances if stones become lodged in the urinary tract, are associated with a urinary infection or cause complications surgery may be needed.
A kidney stone may not cause symptoms until it moves around within your kidney or passes into your ureter the tube connecting the kidney and bladder. At that point, you may experience these signs and symptoms
- Severe pain in the side and back, below the ribs
- Pain that radiates to the lower abdomen and groin
- Pain that comes in waves and fluctuates in intensity
- Pain on urination
- Pink, red or brown urine
- Cloudy or foul-smelling urine
- Nausea and vomiting
- Persistent need to urinate
- Urinating more often than usual
- Fever and chills if an infection is present
- Urinating small amounts
Pain caused by a kidney stone may change for instance, shifting to a different location or increasing in intensity as the stone moves through your urinary tract.

Knowing the type of kidney stone helps determine the cause and may give clues on how to reduce your risk of getting more kidney stones. If possible, try to save your kidney stone if you pass one so that you can bring it with your appointment for analysis.
Types of kidney stones include
- Calcium stones. Most kidney stones are calcium stones, usually in the form of calcium oxalate. Oxalate is a naturally occurring substance found in food and is also made daily by your liver. Some fruits and vegetables, as well as nuts and chocolate, have high oxalate content.
- Dietary factors, high doses of vitamin D, intestinal bypass surgery and several metabolic disorders can increase the concentration of calcium or oxalate in urine.
- Calcium stones may also occur in the form of calcium phosphate. This type of stone is more common in metabolic conditions, such as renal tubular acidosis. It may also be associated with certain migraine headaches or with taking certain seizure medications, such as topiramate (Topamax).
- Struvite stones. Struvite stones form in response to an infection, such as a urinary tract infection. These stones can grow quickly and become quite large, sometimes with few symptoms or little warning.
- Uric acid stones. Uric acid stones can form in people who don’t drink enough fluids or who lose too much fluid, those who eat a high-protein diet, and those who have gout. Certain genetic factors also may increase your risk of uric acid stones.
- Cystine stones. These stones form in people with a hereditary disorder that causes the kidneys to excrete too much of certain amino acids (cystinuria).
Please make an appointment if you have any signs and symptoms that worry you. We will determine how to pass through this together.
Loss of Feeling
or Numbness is most often caused by damage, irritation or compression of nerves.
A single nerve branch, or several nerves, may be affected, as with a slipped disc in the back or carpal tunnel syndrome in the wrist.
Certain diseases, such as diabetes, which can damage the longest, most sensitive nerve fibers (such as those going to your feet), can also cause numbness.

Numbness alone is associated with potentially life-threatening disorders, such as strokes or tumors.
If your loss of feeling or numbness is getting in the way of your daily life, causing pain and not going away please contact Goals Healthcare to diagnose and treat the issue as soon as possible. A variety of tests may be needed to confirm the cause before appropriate treatment can begin.
Lyme Disease (Tick Borne Infections)
Lyme disease is caused by four main species of bacteria. Borrelia burgdorferi and Borrelia mayonii cause Lyme disease in the United States, while Borrelia afzelii and Borrelia garinii are the leading causes in Europe and Asia.
The most common tick-borne illness in these regions, Lyme disease is transmitted by the bite of an infected black-legged tick, commonly known as a deer tick.

The signs and symptoms of Lyme disease vary. They usually appear in stages, but the stages can overlap. A small, red bump, similar to the bump of a mosquito bite, often appears at the site of a tick bite or tick removal and resolves over a few days. This normal occurrence doesn’t indicate Lyme disease. However, these signs and symptoms can occur within a month after you’ve been infected: rash, fever, fatigue, body aches and stiffness
If you need an immediate assessment of your infection please use our telemedicine service or book your visit in office today.
Medical Marijuana
Medical marijuana and natural sources of the cannabis plant have been used in healthcare for hundreds of years. As research continues on the use of marijuana for health care purposes we are learning more about the exact positive effects it may have for a variety of issues and conditions.

Dr. Shanna Levine is certified in understanding the positive uses of medical marijuana and can prescribe for those who present any of the following:
- Post-Traumatic Stress Disorder (PTSD)
- Cancer
- Chronic Pain for More than 3 Months
- Inflammatory Bowel Disease (IBD) (Crohn’s or Ulcerative Colitis)
- Neuropathy
- Epilepsy
- Multiple Sclerosis (MS)
- Spinal Cord Damage with Spasticity
- Amyotrophic Lateral Sclerosis (ALS or Lou Gehrig’s disease)
- Parkinson’s Disease
- Huntington’s Disease
- HIV/AIDS
Odor (Changes in Odor and Odor Control)
Sweating and body odor are facts of life for most people but changes in body odor may be a sign of a medical problem.
Changes in body odor can be noticed when you exercise, when you’re too warm, or when you’re nervous, anxious or under stress.

If you have an unusual change in body odor that you would like to discuss with us please make an appointment today.
We will examine any underlying issues that may be affecting your perspiration and offer different treatment options based on your unique situation.
Opportunistic infections
Opportunistic infections (OIs) are infections that occur more frequently and are more severe in people with weakened immune systems, including people with HIV. Treatments may vary depending on the type of infection.
If you need an immediate assessment of your infection please use our telemedicine service or book your visit in office today.
Osteoarthritis
Osteoarthritis is the most common form of arthritis, affecting millions of people worldwide. It occurs when the protective cartilage on the ends of your bones wears down over time.
Cartilage is a firm, slippery tissue that permits nearly frictionless joint motion. In osteoarthritis, the slick surface of the cartilage becomes rough. Eventually, if the cartilage wears down completely, you may be left with bone rubbing on bone.

Although osteoarthritis can damage any joint in your body, the disorder most commonly affects joints in your hands, knees, hips and spine.
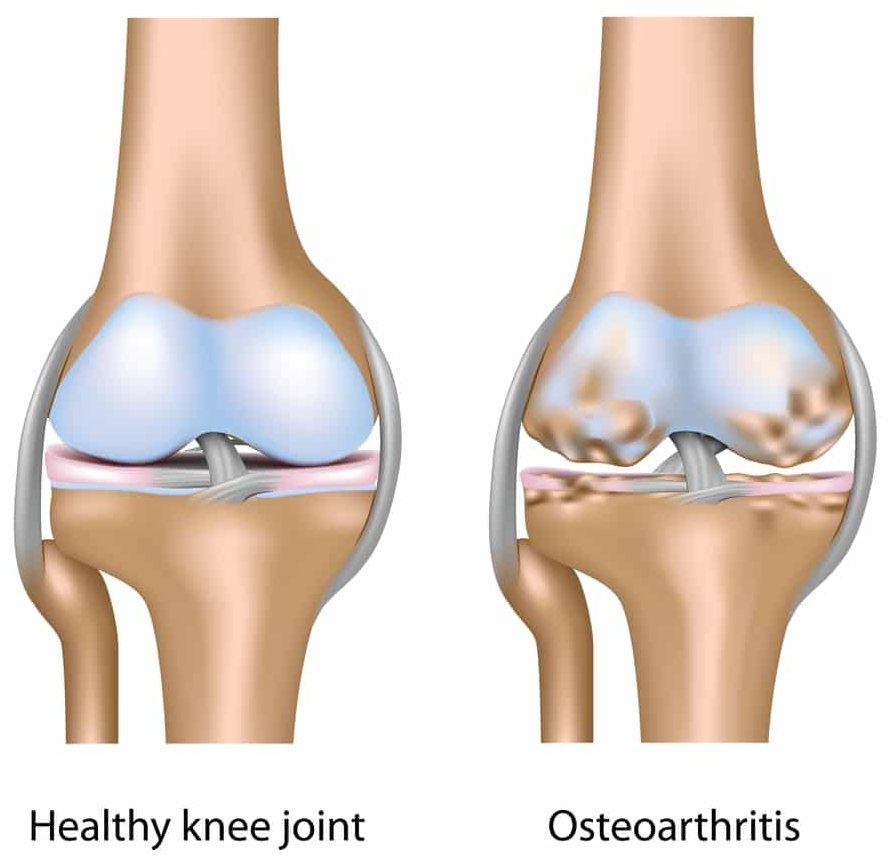
Osteoarthritis symptoms can usually be effectively managed, although the underlying process cannot be reversed.
Signs and symptoms include
- Pain. Your joint may hurt during or after movement.
- Tenderness. Your joint may feel tender when you apply light pressure to it.
- Stiffness. Joint stiffness may be most noticeable when you wake up in the morning or after a period of inactivity.
- Loss of flexibility. You may not be able to move your joint through its full range of motion.
- Grating sensation. You may hear or feel a grating sensation when you use the joint.
- Bone spurs. These extra bits of bone, which feel like hard lumps, may form around the affected joint.
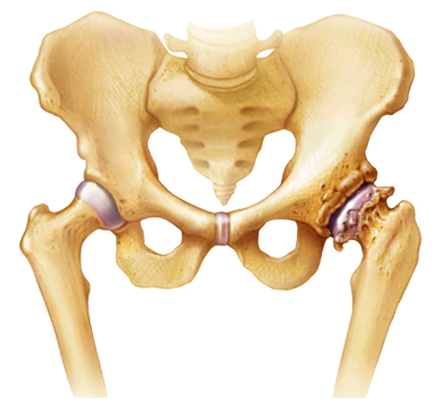
Factors that may increase your risk of osteoarthritis include
- Older age. The risk of osteoarthritis increases with age.
- Sex. Women are more likely to develop osteoarthritis, though it isn’t clear why.
- Obesity. Carrying extra body weight contributes to osteoarthritis in several ways, and the more you weigh, the greater your risk. Increased weight puts added stress on weight-bearing joints, such as your hips and knees. In addition, fat tissue produces proteins that may cause harmful inflammation in and around your joints.
- Joint injuries. Injuries, such as those that occur when playing sports or from an accident, may increase the risk of osteoarthritis. Even injuries that occurred many years ago and seemingly healed can increase your risk of osteoarthritis.
- Certain occupations. If your job includes tasks that place repetitive stress on a particular joint, that joint may eventually develop osteoarthritis.
- Genetics. Some people inherit a tendency to develop osteoarthritis.
- Bone deformities. Some people are born with malformed joints or defective cartilage, which can increase the risk of osteoarthritis.

Osteoarthritis is a degenerative disease that worsens over time.
If you have joint pain or stiffness that doesn’t go away, make an appointment with Goals Healthcare to explore options that are right for You.
Osteoporosis
Osteoporosis causes bones to become weak and brittle. Sometimes so brittle that a fall or even mild stresses such as bending over or coughing can cause a fracture.
Osteoporosis-related fractures most commonly occur in the hip, wrist or spine.

Bone is living tissue that is constantly being broken down and replaced. Osteoporosis occurs when the creation of new bone doesn’t keep up with the removal of old bone.
Osteoporosis affects men and women of all races. But white and Asian women, especially older women who are past menopause are at highest risk. Medications, healthy diet and weight-bearing exercise can help prevent bone loss or strengthen already weak bones.
There typically are no symptoms in the early stages of bone loss. But once your bones have been weakened by osteoporosis, you may have signs and symptoms that include
- Back pain, caused by a fractured or collapsed vertebra
- Loss of height over time
- A stooped posture
- A bone fracture that occurs much more easily than expected
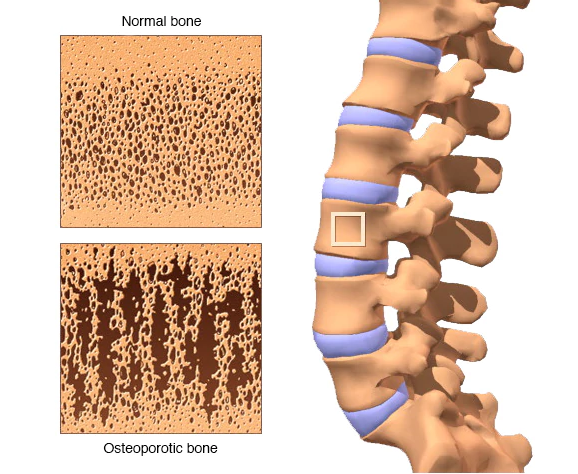
We can put a diet, exercise and medication plan together fit for You. It’s important to be proactive with osteoporosis and Goals Healthcare is here to help you be at your best.
Physicals
Our physicals provide screenings that will reflect our assessment of your specific medical needs and health services, Goals for future visits and progress points to remain on top of your health.
Patients generally receive a physical once a year (Goals Healthcare recommends a full physical examination once a year) and can remain on top of their health.
Many patients are deciding to commit more time and effort into their health by seeing a primary care physician 2-4 times a year.
The bottom line is, everyone is different.
After your initial exam you will receive a full overview of your health, recommendations moving forward (can be additional testing or an immediate plan of action) and personal Goals to reach for.
Own your health. Let’s do it together.
Physicals - Executive Physical
We understand life can get in the way of many things including our health. No problem. Goals Healthcare is here to get you back in charge with our comprehensive exam, the Executive Physical – a program based on current scientific research of best practices customized for You.
For some, receiving an Executive Physical once a year fits their needs. For others it can be years and years, sometimes decades before they receive their first or second Executive Physical. Goals Healthcare is here to ease you back into the process with a comprehensive update on your health.
Our Executive Physical provides screening tests that will reflect our assessment of your specific medical needs and health services, Goals for future visits and progress points to remain on top of your health.
Own your health. Let’s do it together.
Pneumonia
Pneumonia is an infection that inflames the air sacs in one or both lungs.
The air sacs may fill with fluid or pus (purulent material), causing cough with phlegm or pus, fever, chills, and difficulty breathing.
A variety of organisms, including bacteria, viruses and fungi, can cause pneumonia.
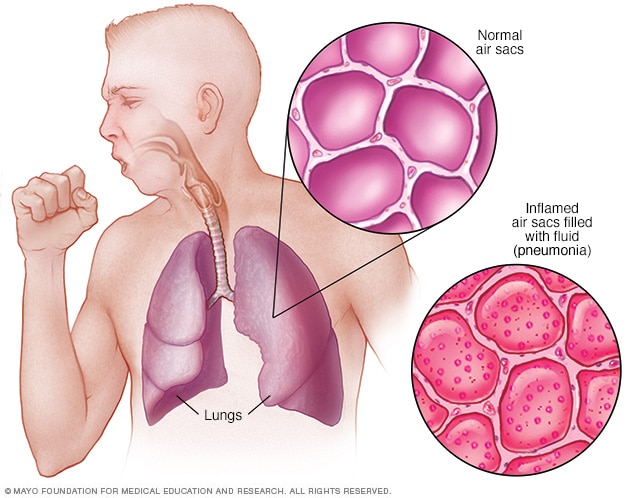
Signs and symptoms of pneumonia may include:
- Chest pain when you breathe or cough
- Confusion or changes in mental awareness (in adults age 65 and older)
- Cough, which may produce phlegm
- Fatigue
- Fever, sweating and shaking chills
- Lower than normal body temperature (in adults older than age 65 and people with weak immune systems)
- Nausea, vomiting or diarrhea
- Shortness of breath
If you feel similar symptoms please contact Goals Healthcare for an immediate assessment.
Pre-and-Post Bariatric Surgery Consult
Weight-loss surgeries make changes to your digestive system to help you lose weight by limiting how much you can eat or by reducing the absorption of nutrients, or both.
Gastric bypass and other weight-loss surgeries are done when diet and exercise haven’t worked or when you have serious health problems because of your weight.
There are many types of weight-loss surgery, known collectively as bariatric surgery. Gastric bypass is one of the most common types of bariatric surgery in the United States.
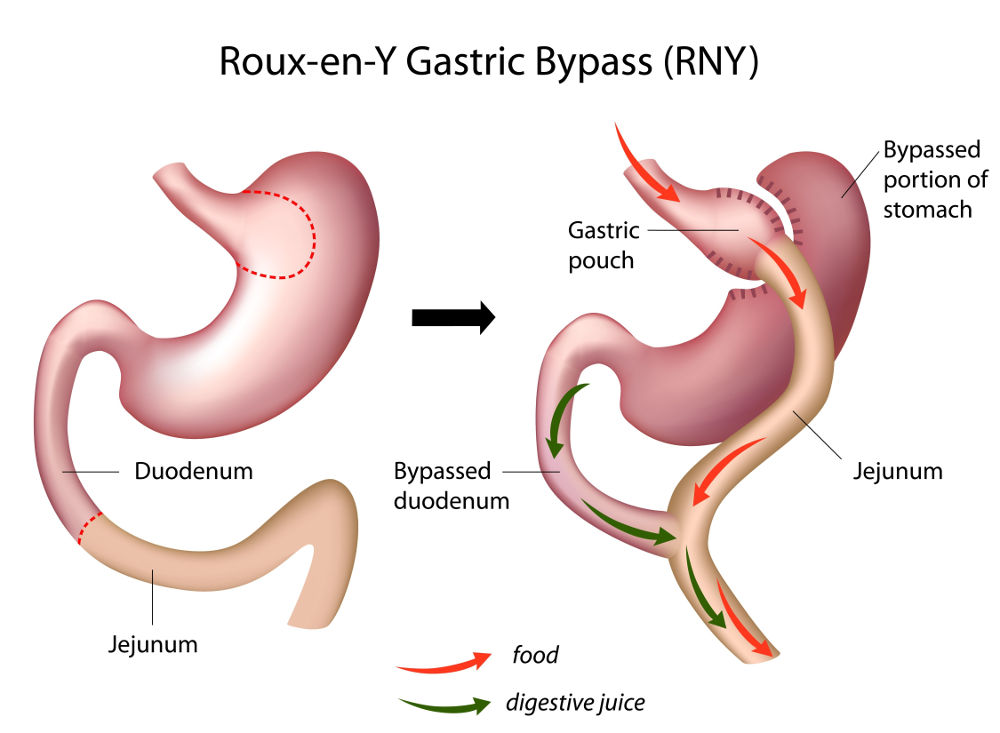
Still, all forms of weight-loss surgery, including gastric bypass, are major procedures that can pose serious risks and side effects. Gastric bypass and other weight-loss surgeries are done only after you’ve tried to lose weight by improving your diet and exercise habits. You must make permanent healthy changes to your diet and get regular exercise to help ensure the long-term success of bariatric surgery.

Weekly, custom, food and diet plans based on your personal weight Goals are provided with our telemedicine memberships pre-and-post bariatric surgery.
Following your surgery we will assist with your immediate recovery needs and long-term Goals of achieving a better quality of life.
Pituitary Gland Issues (Acromegaly)
Acromegaly is a hormonal disorder that develops when your pituitary gland produces too much growth hormone during adulthood. When this happens, your bones increase in size, including those of your hands, feet and face. Acromegaly usually affects middle-aged adults.
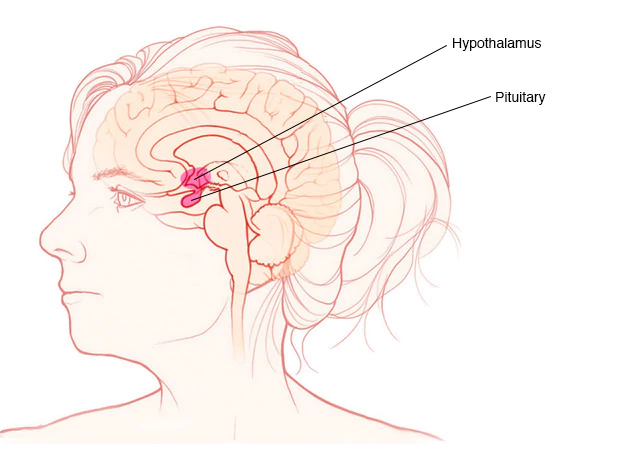
Because acromegaly is uncommon and physical changes occur gradually, the condition often isn’t recognized immediately: sometimes not for years.
If not treated promptly, acromegaly can lead to serious illness and even become life-threatening. However, available treatments for acromegaly can reduce your risk of complications and significantly improve your symptoms, including the enlargement of your features.
One of the most common signs of acromegaly is enlarged hands and feet. People with this disorder often notice that they can no longer put on rings that used to fit and that their shoe size has progressively increased.

Acromegaly may also cause you to experience gradual changes in the shape of your face, such as a protruding lower jaw and brow, an enlarged nose, thickened lips, and wider spacing between your teeth.
Because acromegaly tends to progress slowly, early signs may not be readily apparent for several years. Sometimes, people notice the condition only by comparing old photographs.
Acromegaly may produce the following signs and symptoms, which can vary from one person to another
- Enlarged hands and feet
- Coarsened, enlarged facial features
- Coarse, oily, thickened skin
- Excessive sweating and body odor
- Small outgrowths of skin tissue (skin tags)
- Fatigue and muscle weakness
- A deepened, husky voice due to enlarged vocal cords and sinuses
- Severe snoring due to obstruction of the upper airway
- Impaired vision
- Headaches
- Enlarged tongue
- Pain and limited joint mobility
- Menstrual cycle irregularities in women
- Erectile dysfunction in men
- Enlarged liver, heart, kidneys, spleen and other organs
- Increased chest size (barrel chest)
Treatment focuses on lowering your production of growth hormone, as well as reducing the negative effects of the pituitary gland issues and surrounding tissues.
If you feel you may have a pituitary issue, at your appointment the latest treatment options will be presented to you after diagnosis and any necessary referrals will be provided for local Pituitary Specialists.
Psoriasis
Psoriasis is a common skin condition that speeds up the life cycle of skin cells. It causes cells to build up rapidly on the surface of the skin. The extra skin cells form scales and red patches that are itchy and sometimes painful.
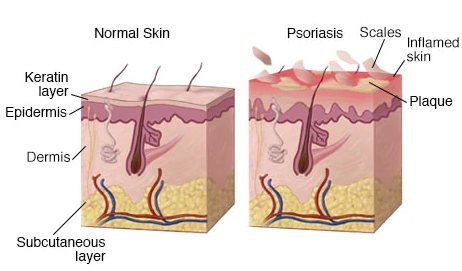
Psoriasis is a chronic disease that often comes and goes. The main goal of treatment is to stop the skin cells from growing so quickly.

Signs and symptoms are different for everyone. Common signs and symptoms include
- Red patches of skin covered with thick, silvery scales
- Small scaling spots (commonly seen in children)
- Dry, cracked skin that may bleed
- Itching, burning or soreness
- Thickened, pitted or ridged nails
- Swollen and stiff joints
Although there is no cure for psoriasis, it is possible to manage symptoms and even keep spots from coming back.

We will break down for you exactly the type of dermatitis you have, and your plan of action to contain the symptoms, redness and eliminate scaly skin.
Make your appointment today for an in-office assessment or get started by using our telemedicine service online.
Respiratory Infections
Respiratory syncytial virus (RSV) causes infections of the lungs and respiratory tract.
Types of upper respiratory infection include the common cold (head cold), the mild flu, tonsillitis, laryngitis, and sinus infection. Of the upper respiratory infection symptoms, the most common is a cough. Lung infections may also lead to a stuffy or runny nose, sore throat, sneezing, achy muscles, and headache.
Otitis is a general term for inflammation or infection of the ear. Sinusitis is an inflammation or swelling of the tissue lining the sinuses. Healthy sinuses are filled with air. But when they become blocked and filled with fluid, germs can grow and cause an infection. Pharyngitis is inflammation of the pharynx, which is in the back of the throat. It’s most often referred to simply as “sore throat.

Make your appointment today for an in-office assessment or get started by using our telemedicine service online.
Skin Infections (Staph, MRSA, Cellulitis)
Have a skin infection or need an evaluation to determine if you have a minor or serious infection do not hesitate to seek medical care.

Staph infections can turn deadly if the bacteria invade deeper into your body, entering your bloodstream, joints, bones, lungs or heart. Staph infections are caused by staphylococcus bacteria, types of germs commonly found on the skin or in the nose of even healthy individuals.
Methicillin-resistant Staphylococcus aureus (MRSA) infection is caused by a type of staph bacteria that’s become resistant to many of the antibiotics used to treat ordinary staph infections.
Cellulitis is a common, potentially serious bacterial skin infection. The affected skin appears swollen and red and is typically painful and warm to the touch. Cellulitis usually affects the skin on the lower legs, but it can occur in the face, arms and other areas. It occurs when a crack or break in your skin allows bacteria to enter.
Staph skin infections, including MRSA, generally start as swollen, painful red bumps that might look like pimples or spider bites. The affected area might be:
- Warm to the touch
- Full of pus or other drainage
- Accompanied by a fever
Make your appointment today for an in-office assessment or get started by using our telemedicine service online.
Shingles
is a viral infection that causes a painful rash. Although shingles can occur anywhere on your body, it most often appears as a single stripe of blisters that wraps around either the left or the right side of your torso.

Shingles is caused by the varicella-zoster virus, the same virus that causes chickenpox.
After you’ve had chickenpox, the virus lies inactive in nerve tissue near your spinal cord and brain. Years later, the virus may reactivate as shingles.
While it isn’t a life-threatening condition, shingles can be very painful. Vaccines can help reduce the risk of shingles, while early treatment can help shorten a shingles infection and lessen the chance of complications.
If you think you may have shingles make an appointment to diagnose and treat your condition as soon as possible.
Sprains, Pains, Bruises and Swelling
Sprains, pains, bruises and swelling is something we all deal with. Knowing what is minor and what is concerning may be difficult to figure out on your own.
A sprain is a stretching or tearing of ligaments — the tough bands of fibrous tissue that connect two bones together in your joints.

If current symptoms are effecting your daily activities and quality of life please contact Goals Healthcare for an immediate assessment and plan of action to get you back to feeling your best.
STD and STI Screenings
Sexually transmitted diseases (STDs) and Sexually transmitted infections (STIs) are generally acquired by sexual contact. The organisms that cause sexually transmitted diseases may pass from person to person in blood, semen, or vaginal and other bodily fluids.

Sometimes these infections can be transmitted nonsexually, such as from mother to infant during pregnancy or childbirth, or through blood transfusions or shared needles.
It’s possible to contract sexually transmitted diseases from people who seem perfectly healthy, and who may not even be aware of the infection. STDs don’t always cause symptoms, which is one of the reasons experts prefer the term “sexually transmitted infections” to “sexually transmitted diseases.”
Sexually transmitted infections (STIs) can have a range of signs and symptoms, including no symptoms. That’s why they may go unnoticed until complications occur or a partner is diagnosed.
Signs and symptoms that might indicate an STI include:
- Sores or bumps on the genitals or in the oral or rectal area
- Painful or burning urination
- Discharge from the penis
- Unusual or odd-smelling vaginal discharge
- Unusual vaginal bleeding
- Pain during sex
- Sore, swollen lymph nodes, particularly in the groin but sometimes more widespread
- Lower abdominal pain
- Fever
- Rash over the trunk, hands or feet
Signs and symptoms may appear a few days after exposure, or it may take years before you have any noticeable problems, depending on the organism.
Because many people in the early stages of an STI experience no symptoms, screening for STIs is important in preventing complications.
Get testing options while learning about several ways to reduce your risk or keep symptoms from returning.
Strep Throat
Strep throat is a bacterial infection that can make your throat feel sore and scratchy.
If untreated, strep throat can cause complications, such as kidney inflammation or rheumatic fever. Rheumatic fever can lead to painful and inflamed joints, a specific type of rash or heart valve damage.

Signs and symptoms of strep throat may include
- Throat pain that usually comes on quickly
- Painful swallowing
- Red and swollen tonsils, sometimes with white patches or streaks of pus
- Tiny red spots on the area at the back of the roof of the mouth (soft or hard palate)
- Swollen, tender lymph nodes in your neck
- Fever
- Headache
- Rash
- Nausea or vomiting, especially in younger children
- Body aches
Strep throat can be extremely painful for some people. Goals Healthcare can help you recover faster when strep throat becomes an issue that will not go away fast enough.
Stroke - Pre and Post Stroke Care and Rehabilitation
A stroke occurs when the blood supply to part of your brain is interrupted or reduced, depriving brain tissue of oxygen and nutrients. Within minutes, brain cells begin to die.
If you feel signs and symptoms of a stroke are affecting you or a loved one please consider seeking care. When possible, pay attention to the signs and symptoms and how they begin or try to remember when they originally began. The length of time they have been present or were present before your stroke occurred.
Understanding when the stroke occurred or what will trigger one can affect your treatment options
- Trouble with speaking and understanding. You may experience confusion. You may slur your words or have difficulty understanding speech.
- Paralysis or numbness of the face, arm or leg. You may develop sudden numbness, weakness or paralysis in your face, arm or leg. This often happens just on one side of your body. Try to raise both your arms over your head at the same time. If one arm begins to fall, you may be having a stroke. Also, one side of your mouth may droop when you try to smile.
- Trouble with seeing in one or both eyes. You may suddenly have blurred or blackened vision in one or both eyes, or you may see double.
- Headache. A sudden, severe headache, which may be accompanied by vomiting, dizziness or altered consciousness, may indicate you’re having a stroke.
- Trouble with walking. You may stumble or experience sudden dizziness, loss of balance or loss of coordination.

To determine the most appropriate treatment for your stroke, the type of stroke you may have and the areas of your brain affected are critical to understanding how to treat signs and symptoms. Ruling out other possible causes, such as a brain tumor or a drug reaction is also equally as important. It may take several tests to determine the cause and additional risks or treatment but Goals Healthcare will be with you throughout the entire process.
Together we will achieve progress!
Sweating (Hyperhidrosis)
Hyperhidrosis (hi-pur-hi-DROE-sis) is abnormally excessive sweating that’s not necessarily related to heat or exercise. You may sweat so much that it soaks through your clothes or drips off your hands.
Besides disrupting normal daily activities, this type of heavy sweating can cause anxiety and depression.

If antiperspirants do not help, sometimes an underlying cause may be found and treated.
If no underlying cause is found Goals Healthcare has the latest medication treatment for excessive sweating.
Or treatment provides a way to block the nerves responsible for the overproduction of sweat.
To learn more about our cutting edge FDA approved hyperhidrosis treatment Click Here.
Thyroid Conditions
Hypothyroidism (underactive thyroid) is a condition in which your thyroid gland doesn’t produce enough of certain important hormones.
Hypothyroidism upsets the normal balance of chemical reactions in your body. It seldom causes symptoms in the early stages, but over time, untreated hypothyroidism can cause a number of health problems, such as obesity, joint pain, infertility and heart disease.

Hypothyroidism signs and symptoms vary depending on the severity of the hormone deficiency and develop slowly, often over a number of years.
- Fatigue
- Increased sensitivity to cold
- Constipation
- Dry skin
- Weight gain
- Puffy face
- Hoarseness
- Muscle weakness
- Elevated blood cholesterol level
- Muscle aches, tenderness and stiffness
- Pain, stiffness or swelling in your joints
- Heavier than normal or irregular menstrual periods
- Thinning hair
- Slowed heart rate
- Depression
- Impaired memory
Hyperthyroidism (overactive thyroid) is a condition in which your thyroid gland produces too much of the hormone thyroxine.
Hyperthyroidism can accelerate your body’s metabolism significantly, causing sudden weight loss, a rapid or irregular heartbeat, sweating, and nervousness or irritability.

Hyperthyroidism can cause a wide variety of signs and symptoms, including
- Sudden weight loss, even when your appetite and the amount and type of food you eat remain the same or even increase
- Rapid heartbeat (tachycardia) commonly more than 100 beats a minute, an irregular heartbeat (arrhythmia) or pounding of your heart (palpitations)
- Increased appetite
- Nervousness, anxiety and irritability
- Tremor usually a fine trembling in your hands and fingers
- Sweating
- Changes in menstrual patterns
- Increased sensitivity to heat
- Changes in bowel patterns, especially more frequent bowel movements
- An enlarged thyroid gland (goiter), which may appear as a swelling at the base of your neck
- Fatigue, muscle weakness
- Difficulty sleeping
- Skin thinning
- Fine, brittle hair
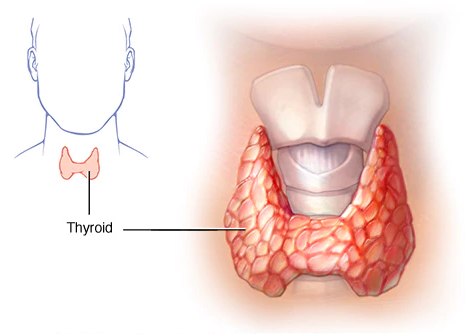
Depending on your thyroid condition we will have a plan ready to improve your daily life. Let’s do this together!
TMJ and Teeth Grinding
TMJ and Teeth Grinding can be painful. TMJ stands for Temporomandibular joint dysfunction and pain.
The temporomandibular (tem-puh-roe-man-DIB-u-lur) joint acts like a sliding hinge, connecting your jawbone to your skull. You have one joint on each side of your jaw. Teeth grinding and TMJ disorders can cause pain in your jaw joint and in the muscles that control jaw movement around it.
Pain and dysfunction from TMJ and Teeth Grinding can lead to
- Clicking and Locking of the Jaw Joint
- Difficulty Biting
- Difficulty Chewing
- Pain
- Teeth Grinding
Goals Healthcare has treatment options that may help reduce the pain and dysfunction associated with teeth grinding and TMJ.
Learn more about Botox® treatment for pain and dysfunction associated with teeth grinding and TMJ
Learn more about Xeomin® treatment for pain and dysfunction associated with teeth grinding and TMJ
Tuberculosis
Tuberculosis (TB) is a potentially serious infectious disease that mainly affects your lungs.
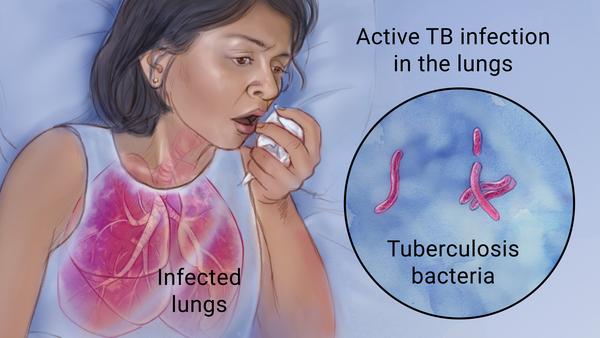
Signs and symptoms of active TB include:
- Coughing that lasts three or more weeks
- Coughing up blood
- Chest pain, or pain with breathing or coughing
- Unintentional weight loss
- Fatigue
- Fever
- Night sweats
- Chills
- Loss of appetite
If you have a fever, unexplained weight loss, drenching night sweats or a persistent cough, make your appointment today for an in-office assessment or get started by using our telemedicine service online.
Vertigo (Dizziness)
One of the most common causes of vertigo is benign paroxysmal positional vertigo (BPPV), the sudden sensation that you’re spinning or that the inside of your head is spinning.
Benign paroxysmal positional vertigo causes brief episodes of mild to intense dizziness.
The signs and symptoms may also include
- A sense that you or your surroundings are spinning or moving (vertigo)
- A loss of balance or unsteadiness
- Nausea
- Vomiting
Benign paroxysmal positional vertigo is usually triggered by specific changes in the position of your head. This might occur when you tip your head up or down, when you lie down, or when you turn over or sit up in bed.
Although benign paroxysmal positional vertigo can be a bothersome problem, it’s rarely serious except when it increases the chance of falls.
Come in today if you feel you may be suffering from vertigo. You can receive effective treatment for benign paroxysmal positional vertigo during your visit.
Vomiting (Excessive)
or Cyclic Vomiting Syndrome is characterized by episodes of severe vomiting that have no apparent cause.
Episodes can last for hours or days and alternate with symptom-free periods. Episodes are similar, meaning that they tend to start at the same time of day, last the same length of time, and occur with the same symptoms and intensity.

Cyclic vomiting syndrome occurs in all age groups, though it often begins when you’re a child.
The symptoms of cyclic vomiting syndrome often begin in the morning. Signs and symptoms include
- Severe vomiting that occurs several times an hour, continues for hours to days, but lasts less than one week
- Three or more separate episodes of vomiting with no apparent cause in the past six months, or five or more episodes occurring at any time
- Severe nausea
- Intense sweating
Other signs and symptoms during a vomiting episode may include
- Abdominal pain
- Diarrhea
- Fever
- Dizziness
- Sensitivity to light
- Headache
- Retching or gagging

The underlying cause of cyclic vomiting syndrome is unknown. Some possible causes include genes, digestive difficulties, nervous system problems and hormone imbalances.
Specific bouts of vomiting may be triggered by
- Colds, allergies or sinus problems
- Emotional stress or excitement, especially in children
- Anxiety or panic attacks, especially in adults
- Foods, such as caffeine, chocolate or cheese
- Overeating, eating right before going to bed or fasting
- Hot weather
- Physical exhaustion
- Exercising too much
- Menstruation
- Motion sickness
We will walk you through the necessary steps to avoid and treat vomiting episodes by pinpointing the underlying issue.
Weight Management
Your weight is a balancing act, and calories are a major part of that equation. Weight comes down to how many calories you take in vs how many calories you burn.

You can do that by reducing extra calories from food and beverages, and increasing calories burned through physical activity.
While that seems simple, it can be challenging mentally and physically to get started.

Together we will implement a practical, effective and sustainable weight management plan. Goals Healthcare is here to assist throughout the process so you don’t have to do it alone. Receive weekly recipes, shopping lists, diet metrics and workout plans.

The key to successful weight management is a commitment to making changes Today. Talk with Goals Healthcare if you’re ready to get started.

Consultations, recipes, diets and workout plans are available in office and online using our telemedicine app.
Wound Care
Our wound care for those with severe or chronic wounds and surgical incisions tries to focus on a whole-body approach to speed the healing process.
A puncture wound, such as from stepping on a nail, doesn’t usually cause excessive bleeding. But these wounds are often deep and can be dangerous because of the risk of infection.

To reduce the risk of infection, prompt treatment and close monitoring for signs of infection are important.
If you need an immediate assessment of your wound please use our telemedicine service online or book your same-day appointment now.
Travel Preparation
Physicals and Medical Clearances
Our physicals and medical clearances for travel preparation will provide screening tests that will reflect our assessment of your specific medical needs and health services, Goals for future visits and a checklist to remain on top of your health during your trip.
Depending on the travel location and your health exam results, vaccinations may be required.
After your exam you will receive an overview of your health and recommendations for your travel preparation (can be additional testing, vaccinations or an immediate plan of action).
Own your health. Let’s do it together.

